| Kidney Res Clin Pract > Volume 42(6); 2023 > Article |
|
Abstract
Background
Methods
Results
Conclusion
Supplementary Materials
Notes
Conflicts of interest
Eun Hui Bae and Soo Wan Kim are the Associate Editors of Kidney Research and Clinical Practice and were not involved in the review process of this article. All authors have no other conflicts of interest to declare.
Funding
This work was supported by the National Research Foundation of Korea (NRF) funded by the Ministry of Science and ICT (MSIT) of the Korean government (NRF-2019R1A2C2086276), by the Basic Science Research Program of the NRF of Korea funded by the Ministry of Education (NRF-2018R1D1A1B07042999), and by a grant (BCRI22080) from Chonnam National University Hospital Biomedical Research Institute.
Figure 1.
Reduction ratios for small and middle uremic toxins in patients who underwent MCO dialysis for 4 weeks, high-flux HD washout for 2 weeks, and then turned to postdilution HDF for 4 weeks.
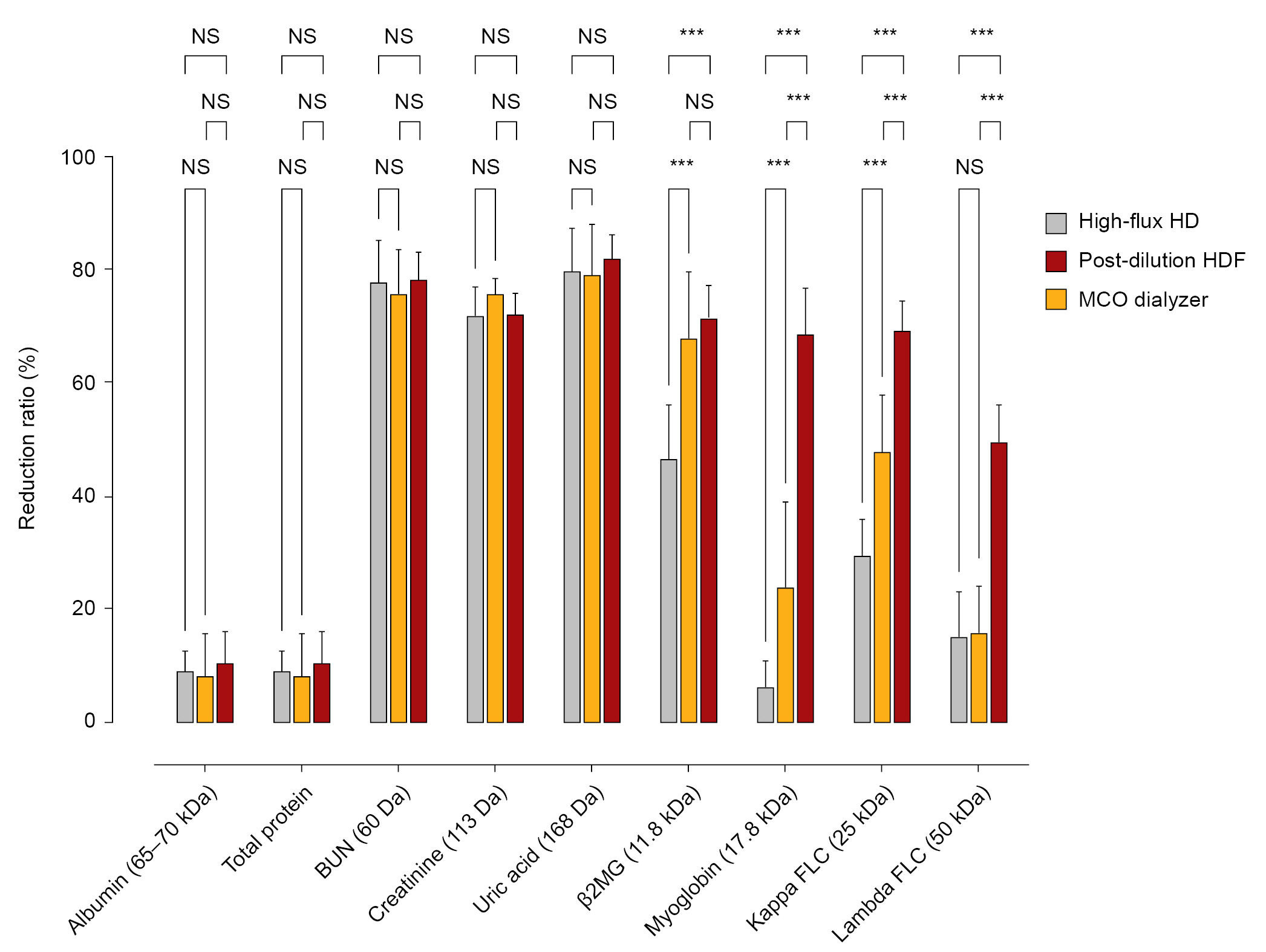
Figure 2.
Serum obtained from patients after completing 4 weeks of MCO dialysis and again after 4 weeks of postdilution HDF was added to human vascular endothelial cells (2.5%) for 16 hours, and the expression of Bax, Bcl-2, and NF-κB p65 was assessed.
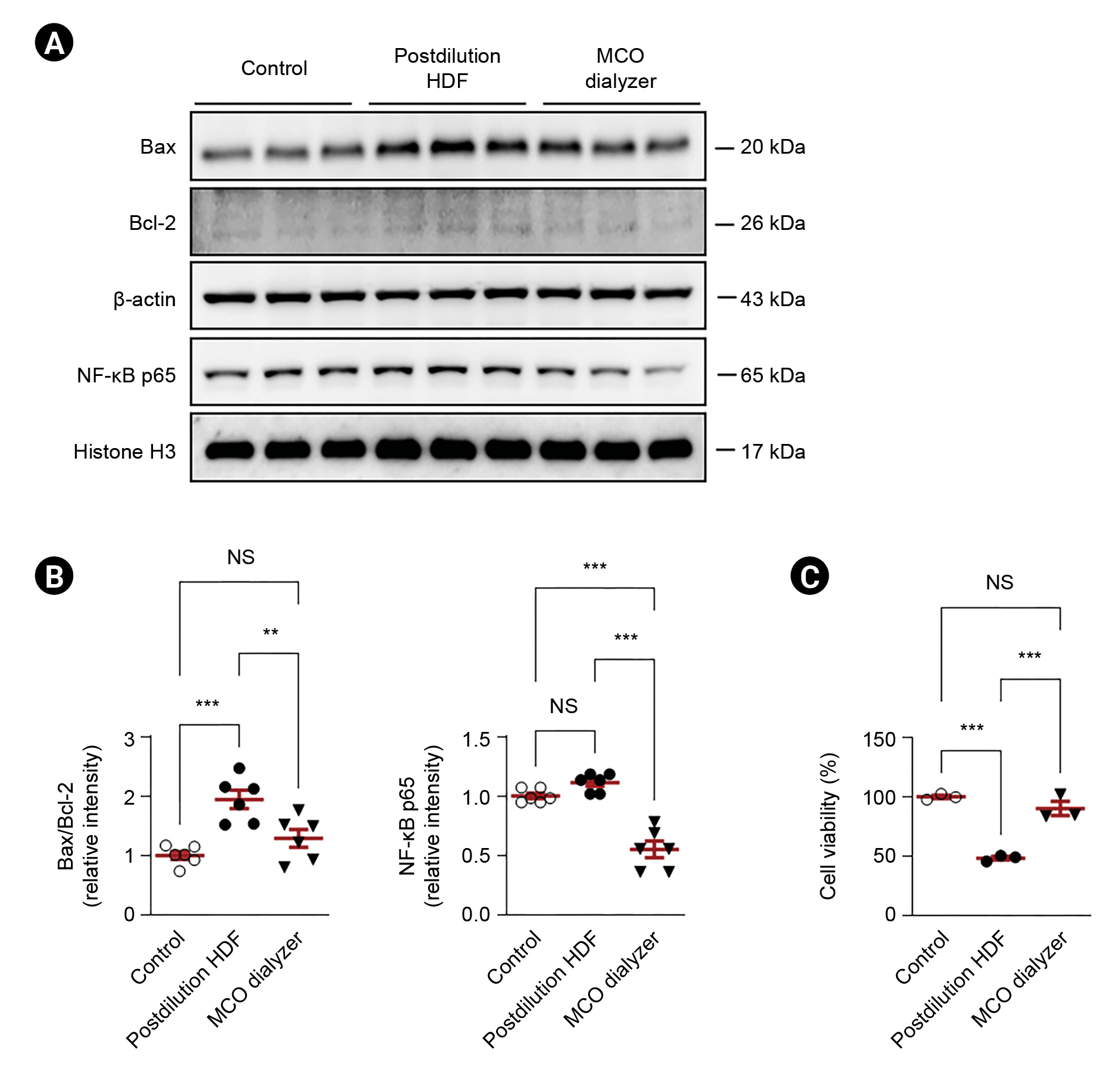
Table 1.
Table 2.
| Variable | High-flux HD, |
Postdilution HDF |
MCO dialysis, | p-valuea | ||
|---|---|---|---|---|---|---|
| 1 wk | Baseline | 4 wk | p-valuea | 4 wk | ||
| Blood flow rate (mL/min) | 270 (250–285) | 270 (250–290) | 270 (250–290) | >0.99 | 250 (220–285) | 0.07 |
| Filtration fraction (%) | NA | 34.0 (32.8–36.5) | 35.0 (33.5–37.0) | 0.39 | NA | |
| Convection volume (L) | NA | 21.0 (18.8–22.9) | 23.3 (20.9–24.3) | 0.13 | NA | |
| Convection volume/BSA (L) | NA | 12.9 (11.7–13.5) | 13.5 (13.2–14.4) | 0.16 | NA | |
Table 3.
| Variable |
High-flux HD |
Postdilution HDF |
MCO dialysis |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Predialysis | Postdialysis | p-valuea | Predialysis | Postdialysis | p-valuea | Predialysis | Postdialysis | p-valuea | |
| Albumin (mg/dL) | 3.5 (3.5–3.85) | 3.2 (3.05–3.60) | 0.008 | 3.7 (3.7–3.9) | 3.5 (3.2–3.7) | 0.02 | 3.8 (3.6–3.9) | 3.4 (3.2–6.5) | 0.008 |
| Total protein (mg/dL) | 6.6 (6.4–6.9) | 6.0 (5.7–6.4) | 0.008 | 6.7 (6.5–7.0) | 6.2 (5.8–6.6) | 0.03 | 6.7 (6.4–7.0) | 6.1 (5.6–6.4) | 0.008 |
| BUN (mg/dL) | 53.5 (32.2–62.0) | 10.4 (9.4–13.0) | 0.008 | 50.4 (33.9–62.2) | 10.9 (9.0–12.1) | 0.008 | 50.8 (35.5–67.3) | 11.4 (6.9–12.5) | 0.008 |
| Creatinine (mg/dL) | 9.15 (7.33–10.17) | 2.51 (2.01–3.11) | 0.008 | 7.97 (6.51–9.80) | 2.36 (2.04–2.69) | 0.008 | 8.24 (6.93–9.47) | 2.21 (1.76–2.65) | 0.008 |
| Uric acid (mg/dL) | 3.8 (3.6–4.9) | 0.8 (0.5–1.0) | 0.008 | 4.0 (2.6–5.1) | 0.7 (0.4–1.1) | 0.008 | 4.7 (3.2–5.7) | 0.8 (0.5–1.1) | 0.008 |
| β2MG, μg/L) | 273,753 (22,546.5–26,008.5) | 12,121.2 (9,586.45–13,951.1) | 0.008 | 21,659.0 (15,043.5–23,918.0) | 6,002.3 (4,614.9–6,875.6) | 0.008 | 23,141.0 (21,705.5–26,281.0) | 6,277.5 (5,217.5–7,518.3) | 0.008 |
| Myoglobin, ng/mL) | 349.0 (215.5–545.5) | 321.5 (197.1–512.9) | 0.01 | 274.0 (238.0–357.5) | 196.0 (144.8–274.2) | 0.02 | 293.0 (211.0–456.0) | 99.1 (50.5–143.1) | 0.008 |
| Kappa FLC (mg/L) | 241.7 (203.0–291.9) | 180.8 (139.6–199.5) | 0.008 | 231.4 (189.8–288.6) | 118.5 (101.1–131.3) | 0.008 | 249.2 (203.0–291.5) | 77.4 (60.3–87.2) | 0.008 |
| Lambda FLC (mg/L) | 188.8 (151.9–243.9) | 158.3 (115.7–214.4) | 0.008 | 186.4 (147.3–255.8) | 155.6 (117.4–222.7) | 0.008 | 192.5 (149.2–262.0) | 100.1 (83.0–117.9) | 0.008 |
Table 4.
| Variablea | High-flux HD | Postdilution HDF | MCO dialysis | p-valueb |
Post hoc analysis |
||
|---|---|---|---|---|---|---|---|
| p-valuec | p-valued | p-valuee | |||||
| Δ of albumin (mg/dL) | 0.31 (0.29–0.37) | 0.42 (0.10–0.54) | 0.32 (0.22–0.56) | 0.97 | 0.48 | 0.67 | 0.95 |
| Δ of total protein (mg/dL) | 0.60 (0.43–0.70) | 0.70 (0.16–1.02) | 0.53 (0.37–0.98) | 0.91 | 0.95 | 0.77 | 0.59 |
| Δ of BUN (mg/dL) | 41.0 (25.3–50.1) | 40.0 (25.0–50.3) | 40.9 (26.0–53.9) | 0.46 | 0.86 | 0.52 | 0.14 |
| Δ of creatinine (mg/dL) | 6.67 (4.89–7.65) | 6.06 (3.88–7.40) | 5.93 (4.92–6.97) | 0.24 | 0.26 | 0.05 | 0.68 |
| Δ of uric acid (mg/dL) | 3.05 (2.77–3.68) | 3.48 (1.86–4.10) | 3.56 (2.70–4.53) | 0.37 | 0.77 | 0.21 | 0.14 |
| Δ of β2MG (μg/L) | 12,052 (8,711–13,512) | 16,318 (8,557–17,474) | 17,173 (14,237–19,771) | <0.001 | 0.099 | <0.001 | 0.02 |
| Δ of myoglobin (ng/mL) | 20.90 (7.90–38.40) | 72.5 (27.5–96.0) | 190.8 (148.7–324.5) | 0.001 | 0.001 | 0.008 | 0.008 |
| Δ of kappa FLC (mg/L) | 64.7 (50.6–97.9) | 107.8 (70.8–148.0) | 174.2 (136.0–208.1) | <0.001 | 0.099 | <0.001 | 0.02 |
| Δ of lambda FLC (mg/L) | 33.0 (18.7–44.4) | 31.5 (15.4–52.3) | 84.3 (71.5–148.2) | 0.001 | 0.81 | 0.001 | 0.002 |
References
- TOOLS
-
METRICS

- ORCID iDs
-
Chang Seong Kim

https://orcid.org/0000-0001-8753-7641Soo Yeon Joo

https://orcid.org/0000-0002-6844-3209Hong Sang Choi

https://orcid.org/0000-0001-8191-4071Eun Hui Bae

https://orcid.org/0000-0003-1727-2822Seong Kwon Ma

https://orcid.org/0000-0002-5758-8189Soo Wan Kim

https://orcid.org/0000-0002-3540-9004 - Related articles



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Supplement table 1
Supplement table 1 Print
Print















