1. Levey A.S., Coresh J., Greene T., Stevens L.A., Zhang Y.L., Hendriksen S., Kusek J.W., Van Lente F.. Chronic Kidney Disease Epidemiology Collaboration: Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate.
Ann Intern Med 145:2006;247ŌĆō254.


2. Cockcroft D.W., Gault M.H.. Prediction of creatinine clearance from serum creatinine.
Nephron 16:1976;31ŌĆō41.


3. Levey A.S., Stevens L.A., Schmid C.H., Zhang Y.L., Castro A.F. 3rd, Feldman H.I., Kusek J.W., Eggers P., Van Lente F., Greene T., Coresh J.. CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration): A new equation to estimate glomerular filtration rate.
Ann Intern Med 150:2009;604ŌĆō612.



4. Imai E., Horio M., Nitta K., Yamagata K., Iseki K., Hara S., Ura N., Kiyohara Y., Hirakata H., Watanabe T., Moriyama T., Ando Y., Inaguma D., Narita I., Iso H., Wakai K., Yasuda Y., Tsukamoto Y., Ito S., Makino H., Hishida A., Matsuo S.. Estimation of glomerular filtration rate by the MDRD study equation modified for Japanese patients with chronic kidney disease.
Clin Exp Nephrol 11:2007;41ŌĆō50.


5. Lee C.S., Cha R.H., Lim Y.H., Kim H., Song K.H., Gu N., Yu K.S., Lim C.S., Han J.S., Kim S., Kim Y.S.. Ethnic coefficients for glomerular filtration rate estimation by the Modification of Diet in Renal Disease study equations in the Korean population.
J Korean Med Sci 25:2010;1616ŌĆō1625.



6. Sj├Čstr├Čm P.A., Odlind B.G., Wolgast M.. Extensive tubular secretion and reabsorption of creatinine in humans.
Scand J Urol Nephrol 22:1988;129ŌĆō131.


7. Shemesh O., Golbetz H., Kriss J.P., Myers B.D.. Limitations of creatinine as a filtration marker in glomerulopathic patients.
Kidney Int 28:1985;830ŌĆō838.


8. Abrahamson M., Olafsson I., Palsdottir A., Ulvsb├żck M., Lundwall A., Jensson O., Grubb A.. Structure and expression of the human cystatin C gene.
Biochem J 268:1990;287ŌĆō294.



9. Grubb A., Simonsen O., Sturfelt G., Truedsson L., Thysell H.. Serum concentration of cystatin C, factor D and beta 2-microglobulin as a measure of glomerular filtration rate.
Acta Med Scand 218:1985;499ŌĆō503.


10. Simonsen O., Grubb A., Thysell H.. The blood serum concentration of cystatin C (gamma-trace) as a measure of the glomerular filtration rate.
Scand J Clin Lab Invest 45:1985;97ŌĆō101.


11. Zhang Z., Lu B., Sheng X., Jin N.. Cystatin C in prediction of acute kidney injury: a systemic review and meta-analysis.
Am J Kidney Dis 58:2011;356ŌĆō365.

12. Zappitelli M., Krawczeski C.D., Devarajan P., Wang Z., Sint K., Thiessen-Philbrook H., Li S., Bennett M.R., Ma Q., Shlipak M.G., Garg A.X., Parikh C.R.. TRIBE-AKI consortium: Early postoperative serum cystatin C predicts severe acute kidney injury following pediatric cardiac surgery.
Kidney Int 80:2011;655ŌĆō662.

13. Zahran A., El-Husseini A., Shoker A.. Can cystatin C replace creatinine to estimate glomerular filtration rate? A literature review.
Am J Nephrol 27:2007;197ŌĆō205.


14. Dharnidharka V.R., Kwon C., Stevens G.. Serum cystatin C is superior to serum creatinine as a marker of kidney function: a meta-analysis.
Am J Kidney Dis 40:2002;221ŌĆō226.


15. Han K.H., Han S.Y., Kang Y.S., Cha D.R.. Serum cystatin C concentration compared with serum creatinine concentration as a marker of glomerular filtration rate. Korean J Nephrol 25:2006;737ŌĆō744.
16. Larsson A., Malm J., Grubb A., Hansson L.O.. Calculation of glomerular filtration rate expressed in mL/min from plasma cystatin C values in mg/L.
Scand J Clin Lab Invest 64:2004;25ŌĆō30.


17. Hoek F.J., Kemperman F.A., Krediet R.T.. A comparison between cystatin C, plasma creatinine and the Cockcroft and Gault formula for the estimation of glomerular filtration rate.
Nephrol Dial Transplant 18:2003;2024ŌĆō2031.


18. Le Bricon T., Thervet E., Froissart M., Benlakehal M., Bousquet B., Legendre C., Erlich D.. Plasma cystatin C is superior to 24-h creatinine clearance and plasma creatinine for estimation of glomerular filtration rate 3 months after kidney transplantation.
Clin Chem 46:2000;1206ŌĆō1207.


19. Filler G., Lepage N.. Should the Schwartz formula for estimation of GFR be replaced by cystatin C formula?
Pediatr Nephrol 18:2003;981ŌĆō985.


20. Sj├Čstr├Čm P., Tidman M., Jones I.. Determination of the production rate and non-renal clearance of cystatin C and estimation of the glomerular filtration rate from the serum concentration of cystatin C in humans.
Scand J Clin Lab Invest 65:2005;111ŌĆō124.


21. Fricker M., Wiesli P., Br├żndle M., Schwegler B., Schmid C.. Impact of thyroid dysfunction on serum cystatin C.
Kidney Int 63:2003;1944ŌĆō1947.


22. Knight E.L., Verhave J.C., Spiegelman D., Hillege H.L., de Zeeuw D., Curhan G.C., de Jong P.E.. Factors influencing serum cystatin C levels other than renal function and the impact on renal function measurement.
Kidney Int 65:2004;1416ŌĆō1421.


23. Stevens L.A., Schmid C.H., Greene T., Li L., Beck G.J., Joffe M.M., Froissart M., Kusek J.W., Zhang Y.L., Coresh J., Levey A.S.. Factors other than glomerular filtration rate affect serum cystatin C levels.
Kidney Int 75:2009;652ŌĆō660.


24. Gates G.F.. Computation of glomerular filtration rate with Tc-99m DTPA: an in-house computer program.
J Nucl Med 25:1984;613ŌĆō618.

25. http://www.kidney.org/professionals/KDOQI/guidelines_ckd.
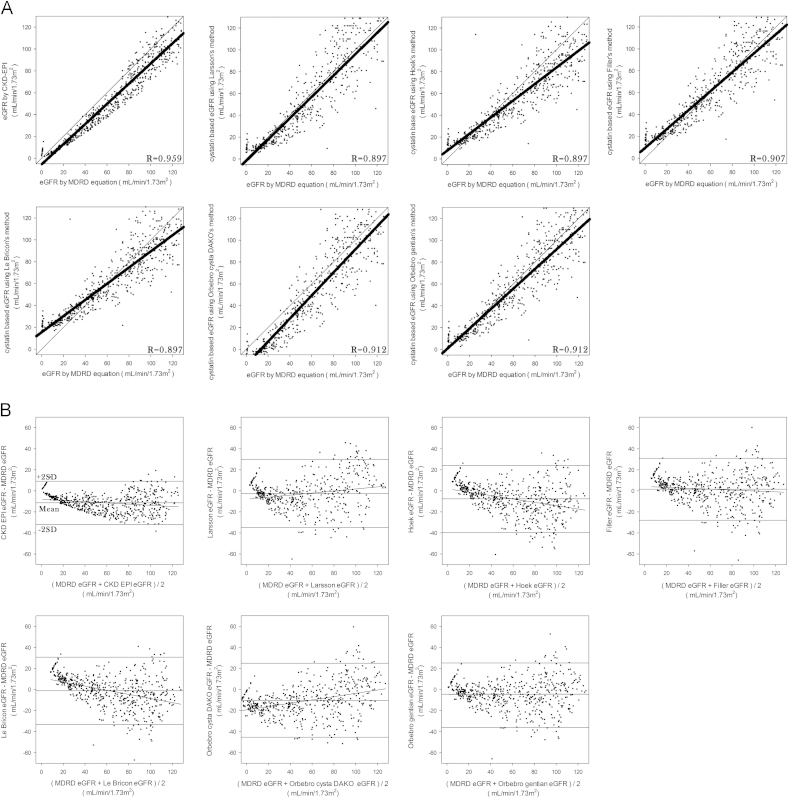
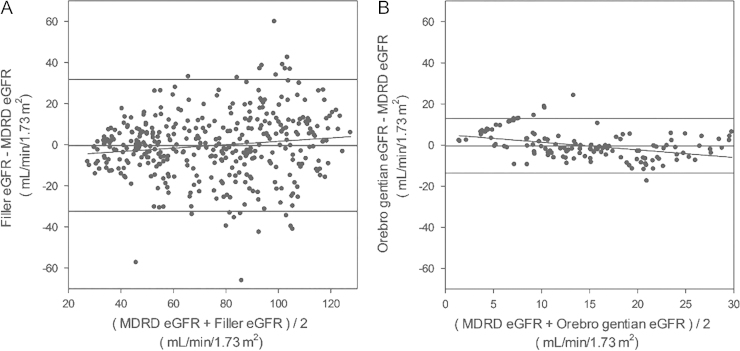
26. Bland J.M., Altman D.G.. Statistical methods for assessing agreement between two methods of clinical measurement.
Lancet 8:1986;307ŌĆō310.

27. Rule A.D., Larson T.S., Bergstralh E.J., Slezak J.M., Jacobsen S.J., Cosio F.G.. Using serum creatinine to estimate glomerular filtration rate: accuracy in good health and in chronic kidney disease.
Ann Intern Med 141:2004;929ŌĆō937.


28. Hallan S., Asberg A., Lindberg M., Johnsen H.. Validation of the Modification of Diet in Renal Disease formula for estimating GFR with special emphasis on calibration of the serum creatinine assay.
Am J Kidney Dis 44:2004;84ŌĆō93.


29. Uemura O., Ushijima K., Nagai T., Yamada T., Yamakawa S., Hibi Y., Hayakawa H., Nabeta Y., Shinkai Y., Koike K., Kuwabara M.. Measurements of serum cystatin C concentrations underestimate renal dysfunction in pediatric patients with chronic kidney disease.
Clin Exp Nephrol 15:2011;535ŌĆō538.


30. Tidman M., Sj├Čstr├Čm P., Jones I.. A comparison of GFR estimating formulae based upon s-cystatin C and s-creatinine and a combination of the two.
Nephrol Dial Transplant 23:2008;154ŌĆō160.


31. Comprehensive Clinical Nephrology.
32. Randers E., Erlandsen E.J., Pedersen O.L., Hasling C., Danielsen H.. Serum cystatin C as an endogenous parameter of the renal function in patients with normal to moderately impaired kidney function.
Clin Nephrol 54:2000;203ŌĆō209.

33. Coll E., Botey A., Alvarez L., Poch E., Quint├│ L., Saurina A., Vera M., Piera C., Darnell A.. Serum cystatin C as a new marker for noninvasive estimation of glomerular filtration rate and as a marker for early renal impairment.
Am J Kidney Dis 36:2000;29ŌĆō34.







 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print
















