1. Ballermann BJ. Glomerular endothelial cell differentiation.
Kidney Int 2005;67:1668–1671.


2. Lennon R, Byron A, Humphries JD, et al. Global analysis reveals the complexity of the human glomerular extracellular matrix.
J Am Soc Nephrol 2014;25:939–951.



3. Sison K, Eremina V, Baelde H, et al. Glomerular structure and function require paracrine, not autocrine, VEGF-VEGFR-2 signaling.
J Am Soc Nephrol 2010;21:1691–1701.



4. Kim SH, Turnbull J, Guimond S. Extracellular matrix and cell signalling: the dynamic cooperation of integrin, proteoglycan and growth factor receptor.
J Endocrinol 2011;209:139–151.


5. Mause SF, Weber C. Microparticles: protagonists of a novel communication network for intercellular information exchange.
Circ Res 2010;107:1047–1057.


6. Abrahamson DR. Glomerulogenesis in the developing kidney.
Semin Nephrol 1991;11:375–389.

7. Eremina V, Sood M, Haigh J, et al. Glomerular-specific alterations of VEGF-A expression lead to distinct congenital and acquired renal diseases.
J Clin Invest 2003;111:707–716.



8. Eremina V, Jefferson JA, Kowalewska J, et al. VEGF inhibition and renal thrombotic microangiopathy.
N Engl J Med 2008;358:1129–1136.



9. Jin J, Sison K, Li C, et al. Soluble FLT1 binds lipid microdomains in podocytes to control cell morphology and glomerular barrier function.
Cell 2012;151:384–399.


10. Maynard SE, Min JY, Merchan J, et al. Excess placental soluble fms-like tyrosine kinase 1 (sFlt1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia.
J Clin Invest 2003;111:649–658.



11. Carmeliet P, Ferreira V, Breier G, et al. Abnormal blood vessel development and lethality in embryos lacking a single VEGF allele.
Nature 1996;380:435–439.



12. Hertig A, Berkane N, Lefevre G, et al. Maternal serum sFlt1 concentration is an early and reliable predictive marker of preeclampsia.
Clin Chem 2004;50:1702–1703.



13. Izzedine H, Soria JC, Escudier B. Proteinuria and VEGF-targeted therapies: an underestimated toxicity?
J Nephrol 2013;26:807–810.


14. Cooper ME, Vranes D, Youssef S, et al. Increased renal expression of vascular endothelial growth factor (VEGF) and its receptor VEGFR-2 in experimental diabetes.
Diabetes 1999;48:2229–2239.



15. Sung SH, Ziyadeh FN, Wang A, Pyagay PE, Kanwar YS, Chen S. Blockade of vascular endothelial growth factor signaling ameliorates diabetic albuminuria in mice.
J Am Soc Nephrol 2006;17:3093–3104.


16. Veron D, Reidy KJ, Bertuccio C, et al. Overexpression of VEGF-A in podocytes of adult mice causes glomerular disease.
Kidney Int 2010;77:989–999.


19. Lindenmeyer MT, Kretzler M, Boucherot A, et al. Interstitial vascular rarefaction and reduced VEGF-A expression in human diabetic nephropathy.
J Am Soc Nephrol 2007;18:1765–1776.


20. Nitta K, Uchida K, Kimata N, et al. Increased serum levels of vascular endothelial growth factor in human crescentic glomerulonephritis.
Clin Nephrol 1999;52:76–82.

21. Thomas S, Vanuystel J, Gruden G, et al. Vascular endothelial growth factor receptors in human mesangium in vitro and in glomerular disease.
J Am Soc Nephrol 2000;11:1236–1243.


22. Pilmore HL, Eris JM, Painter DM, Bishop GA, McCaughan GW. Vascular endothelial growth factor expression in human chronic renal allograft rejection.
Transplantation 1999;67:929–933.


23. Malmström NK, Kallio EA, Rintala JM, et al. Vascular endothelial growth factor in chronic rat allograft nephropathy.
Transpl Immunol 2008;19:136–144.


24. Lemström KB, Krebs R, Nykänen AI, et al. Vascular endothelial growth factor enhances cardiac allograft arteriosclerosis.
Circulation 2002;105:2524–2530.


25. Hellström M, Kalén M, Lindahl P, Abramsson A, Betsholtz C. Role of PDGF-B and PDGFR-beta in recruitment of vascular smooth muscle cells and pericytes during embryonic blood vessel formation in the mouse.
Development 1999;126:3047–3055.

26. Ozdemir BH, Ozdemir FN, Haberal N, Emiroglu R, Demirhan B, Haberal M. Vascular endothelial growth factor expression and cyclosporine toxicity in renal allograft rejection.
Am J Transplant 2005;5:766–774.


27. Karet FE, Davenport AP. Localization of endothelin peptides in human kidney.
Kidney Int 1996;49:382–387.


28. Sakurai T, Yanagisawa M, Takuwa Y, et al. Cloning of a cDNA encoding a non-isopeptide-selective subtype of the endothelin receptor.
Nature 1990;348:732–735.



29. Kuc R, Davenport AP. Comparison of endothelin-A and endothelin-B receptor distribution visualized by radioligand binding versus immunocytochemical localization using subtype selective antisera.
J Cardiovasc Pharmacol 2004;44 Suppl 1:S224–S226.


30. Kelland NF, Kuc RE, McLean DL, et al. Endothelial cell-specific ETB receptor knockout: autoradiographic and histological characterisation and crucial role in the clearance of endothelin-1.
Can J Physiol Pharmacol 2010;88:644–651.


31. Gariepy CE, Ohuchi T, Williams SC, Richardson JA, Yanagisawa M. Salt-sensitive hypertension in endothelin-B receptor-deficient rats.
J Clin Invest 2000;105:925–933.



32. Rebibou JM, He CJ, Delarue F, et al. Functional endothelin 1 receptors on human glomerular podocytes and mesangial cells.
Nephrol Dial Transplant 1992;7:288–292.


33. Lenoir O, Milon M, Virsolvy A, et al. Direct action of endothelin-1 on podocytes promotes diabetic glomerulosclerosis.
J Am Soc Nephrol 2014;25:1050–1062.



34. Yuan M, Tan Y, Wang Y, Wang SX, Yu F, Zhao MH. The associations of endothelial and podocyte injury in proliferative lupus nephritis: from observational analysis to in vitro study.
Lupus 2019;28:347–358.



35. Daehn I, Casalena G, Zhang T, et al. Endothelial mitochondrial oxidative stress determines podocyte depletion in segmental glomerulosclerosis.
J Clin Invest 2014;124:1608–1621.



36. Ebefors K, Wiener RJ, Yu L, et al. Endothelin receptor-A mediates degradation of the glomerular endothelial surface layer via pathologic crosstalk between activated podocytes and glomerular endothelial cells.
Kidney Int 2019;96:957–970.



37. Kohan DE. Production of endothelin-1 by rat mesangial cells: regulation by tumor necrosis factor.
J Lab Clin Med 1992;119:477–484.

38. Lamas S, Michel T, Collins T, Brenner BM, Marsden PA. Effects of interferon-gamma on nitric oxide synthase activity and endothelin-1 production by vascular endothelial cells.
J Clin Invest 1992;90:879–887.



39. Zoja C, Orisio S, Perico N, et al. Constitutive expression of endothelin gene in cultured human mesangial cells and its modulation by transforming growth factor-beta, thrombin, and a thromboxane A2 analogue.
Lab Invest 1991;64:16–20.

40. Marsden PA, Dorfman DM, Collins T, Brenner BM, Orkin SH, Ballermann BJ. Regulated expression of endothelin 1 in glomerular capillary endothelial cells.
Am J Physiol 1991;261:F117–F125.


41. Cybulsky AV, Stewart DJ, Cybulsky MI. Glomerular epithelial cells produce endothelin-1.
J Am Soc Nephrol 1993;3:1398–1404.


42. Horie M, Uchida S, Yanagisawa M, Matsushita Y, Kurokawa K, Ogata E. Mechanisms of endothelin-1 mRNA and peptides induction by TGF-beta and TPA in MDCK cells.
J Cardiovasc Pharmacol 1991;17 Suppl 7:S222–S225.

43. Deng DX, Jiang J, Garcia B, Zhong R, Chakrabarti S. Endothelin-1, endothelin-3 and their receptors (endothelin(A) and endothelin(B)) in chronic renal transplant rejection in rats.
Transpl Int 2000;13:175–182.


44. Siddiqui I, Khan ZA, Lian D, et al. Endothelin-mediated oncofetal fibronectin expression in chronic allograft nephropathy.
Transplantation 2006;82:406–414.


45. Nakatani T, Tanabe S, Han YS, et al. Enhanced expression of endothelin-A receptor in human transplant renal arteriosclerosis.
Int J Mol Med 2003;11:153–156.


46. Kanetsuna Y, Takahashi K, Nagata M, et al. Deficiency of endothelial nitric-oxide synthase confers susceptibility to diabetic nephropathy in nephropathy-resistant inbred mice.
Am J Pathol 2007;170:1473–1484.



47. Gu X, Herrera GA. Expression of eNOS in kidneys from hypertensive patients.
Int J Nephrol Renovasc Dis 2010;3:11–19.



48. Ueda S, Ozawa S, Mori K, et al. ENOS deficiency causes podocyte injury with mitochondrial abnormality.
Free Radic Biol Med 2015;87:181–192.


49. Sun YB, Qu X, Zhang X, Caruana G, Bertram JF, Li J. Glomerular endothelial cell injury and damage precedes that of podocytes in adriamycin-induced nephropathy.
PLoS One 2013;8:e55027.



50. Mooyaart AL, Valk EJ, van Es LA, et al. Genetic associations in diabetic nephropathy: a meta-analysis.
Diabetologia 2011;54:544–553.


51. Collino F, Bussolati B, Gerbaudo E, et al. Preeclamptic sera induce nephrin shedding from podocytes through endothelin-1 release by endothelial glomerular cells.
Am J Physiol Renal Physiol 2008;294:F1185–F1194.


52. Sud N, Black SM. Endothelin-1 impairs nitric oxide signaling in endothelial cells through a protein kinase Cdelta-dependent activation of STAT3 and decreased endothelial nitric oxide synthase expression.
DNA Cell Biol 2009;28:543–553.


53. Jeansson M, Gawlik A, Anderson G, et al. Angiopoietin-1 is essential in mouse vasculature during development and in response to injury.
J Clin Invest 2011;121:2278–2289.



54. Dessapt-Baradez C, Woolf AS, White KE, et al. Targeted glomerular angiopoietin-1 therapy for early diabetic kidney disease.
J Am Soc Nephrol 2014;25:33–42.


55. Yuan HT, Tipping PG, Li XZ, Long DA, Woolf AS. Angiopoietin correlates with glomerular capillary loss in anti-glomerular basement membrane glomerulonephritis.
Kidney Int 2002;61:2078–2089.


56. Davis B, Dei Cas A, Long DA, et al. Podocyte-specific expression of angiopoietin-2 causes proteinuria and apoptosis of glomerular endothelia.
J Am Soc Nephrol 2007;18:2320–2329.


57. Molnar MZ, Kümpers P, Kielstein JT, et al. Circulating Angiopoietin-2 levels predict mortality in kidney transplant recipients: a 4-year prospective case-cohort study.
Transpl Int 2014;27:541–552.


58. Ma X, Lu YP, Yang L, et al. Expressions of Angiopoietin-1, Angiopoietin-2, and Tie2 and their roles in rat renal allografts with chronic allograft nephropathy.
Transplant Proc 2008;40:2795–2799.


59. Thamm K, Njau F, Van Slyke P, et al. Pharmacological Tie2 activation in kidney transplantation.
World J Transplant 2016;6:573–582.



60. Sierro F, Biben C, Martínez-Muñoz L, et al. Disrupted cardiac development but normal hematopoiesis in mice deficient in the second CXCL12/SDF-1 receptor, CXCR7.
Proc Natl Acad Sci U S A 2007;104:14759–14764.



61. Takabatake Y, Sugiyama T, Kohara H, et al. The CXCL12 (SDF-1)/CXCR4 axis is essential for the development of renal vasculature.
J Am Soc Nephrol 2009;20:1714–1723.



62. Haege S, Einer C, Thiele S, et al. CXC chemokine receptor 7 (CXCR7) regulates CXCR4 protein expression and capillary tuft development in mouse kidney.
PLoS One 2012;7:e42814.



64. Hoffmann U, Banas B, Krüger B, et al. SDF-1 expression is elevated in chronic human renal allograft rejection.
Clin Transplant 2006;20:712–718.


65. Tang H, Xu Y, Zhang Z, et al. SDF‑1/CXCR4 induces epithelial‑mesenchymal transition through activation of the Wnt/β‑catenin signaling pathway in rat chronic allograft nephropathy.
Mol Med Rep 2019;19:3696–3706.



66. Xu Y, Zhang Q, Xue W, et al. CXC chemokine receptor 4 (CXCR4) antagonist, a novel pathway to prevent chronic allograft nephropathy.
Ann Transplant 2016;21:728–734.


67. Gao C, Huan J. SDF-1 plays a key role in chronic allograft nephropathy in rats.
Transplant Proc 2008;40:1674–1678.


68. Togel FE, Westenfelder C. Role of SDF-1 as a regulatory chemokine in renal regeneration after acute kidney injury.
Kidney Int Suppl (2011) 2011;1:87–89.



69. Narazaki M, Yasukawa K, Saito T, et al. Soluble forms of the interleukin-6 signal-transducing receptor component gp130 in human serum possessing a potential to inhibit signals through membrane-anchored gp130.
Blood 1993;82:1120–1126.



70. Moreno Velásquez I, Golabkesh Z, Källberg H, Leander K, de Faire U, Gigante B. Circulating levels of interleukin 6 soluble receptor and its natural antagonist, sgp130, and the risk of myocardial infarction.
Atherosclerosis 2015;240:477–481.


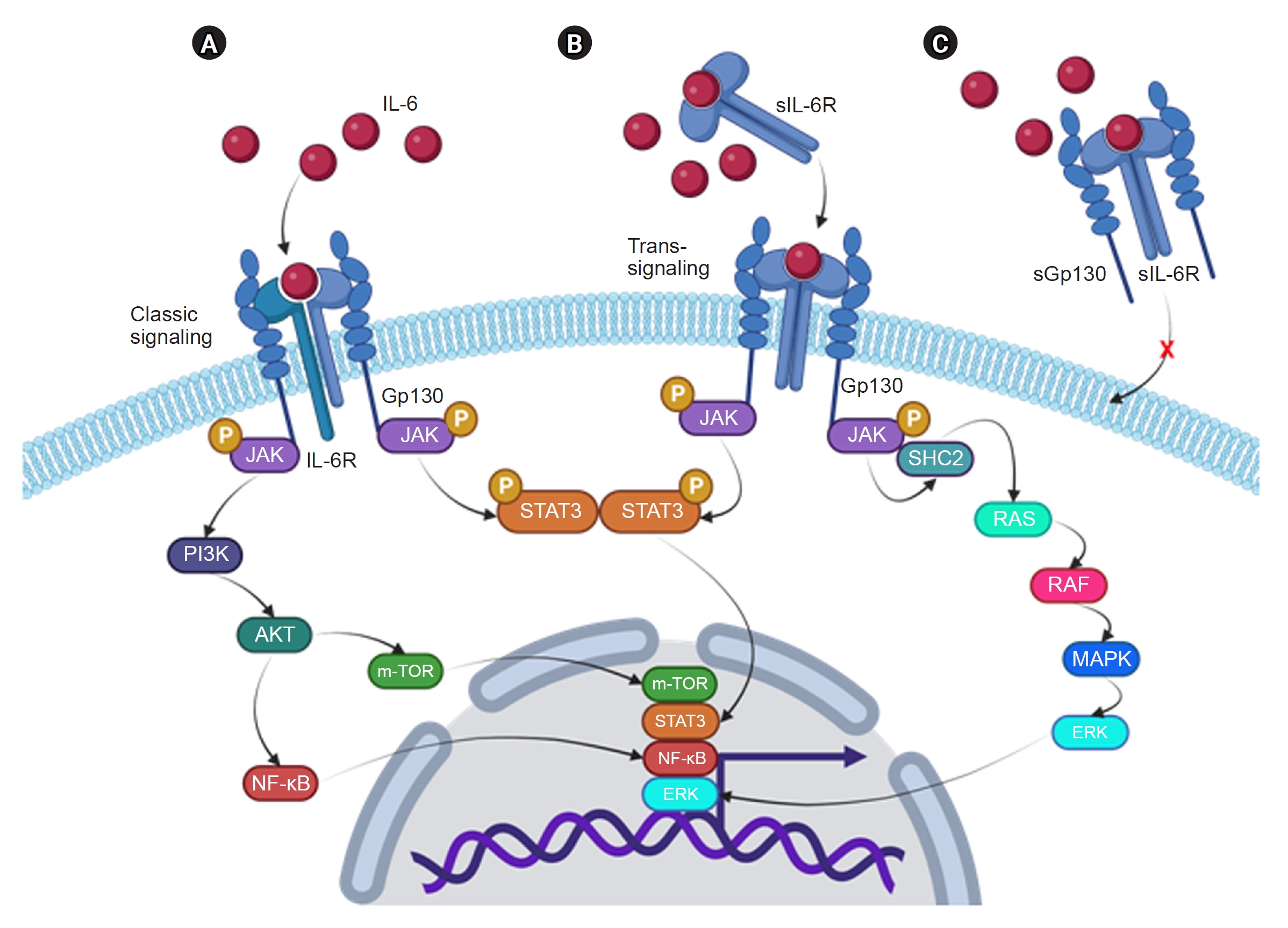
71. Scheller J, Chalaris A, Schmidt-Arras D, Rose-John S. The pro- and anti-inflammatory properties of the cytokine interleukin-6.
Biochim Biophys Acta 2011;1813:878–888.


72. Malchow S, Thaiss W, Jänner N, et al. Essential role of neutrophil mobilization in concanavalin A-induced hepatitis is based on classic IL-6 signaling but not on IL-6 trans-signaling.
Biochim Biophys Acta 2011;1812:290–301.


73. Su H, Lei CT, Zhang C. Interleukin-6 signaling pathway and its role in kidney disease: an update.
Front Immunol 2017;8:405.



74. Wassmann S, Stumpf M, Strehlow K, et al. Interleukin-6 induces oxidative stress and endothelial dysfunction by overexpression of the angiotensin II type 1 receptor.
Circ Res 2004;94:534–541.


75. Wang S, Jiang J, Guan Q, et al. Reduction of Foxp3-expressing regulatory T cell infiltrates during the progression of renal allograft rejection in a mouse model.
Transpl Immunol 2008;19:93–102.


76. Wang H, Guan Q, Lan Z, et al. Prolonged renal allograft survival by donor interleukin-6 deficiency: association with decreased alloantibodies and increased intragraft T regulatory cells.
Am J Physiol Renal Physiol 2012;302:F276–F283.


77. Tse GH, Johnston CJ, Kluth D, et al. Intrarenal B cell cytokines promote transplant fibrosis and tubular atrophy.
Am J Transplant 2015;15:3067–3080.


78. Waiser J, Budde K, Katalinic A, Kuerzdörfer M, Riess R, Neumayer HH. Interleukin-6 expression after renal transplantation.
Nephrol Dial Transplant 1997;12:753–759.


79. Raasveld MH, Weening JJ, Kerst JM, Surachno S, ten Berge RJ. Local production of interleukin-6 during acute rejection in human renal allografts.
Nephrol Dial Transplant 1993;8:75–78.


80. Kawai T, Sachs DH, Sykes M, Cosimi AB; Immune Tolerance Network. HLA-mismatched renal transplantation without maintenance immunosuppression.
N Engl J Med 2013;368:1850–1852.



81. Poppelaars F, Gaya da Costa M, Eskandari SK, Damman J, Seelen MA. Donor genetic variants in interleukin-6 and interleukin-6 receptor associate with biopsy-proven rejection following kidney transplantation.
Sci Rep 2021;11:16483.



82. Nechemia-Arbely Y, Barkan D, Pizov G, et al. IL-6/IL-6R axis plays a critical role in acute kidney injury.
J Am Soc Nephrol 2008;19:1106–1115.



84. Ragni E, Banfi F, Barilani M, et al. Extracellular vesicle-shuttled mRNA in mesenchymal stem cell communication.
Stem Cells 2017;35:1093–1105.



86. Medica D, Franzin R, Stasi A, et al. Extracellular vesicles derived from endothelial progenitor cells protect human glomerular endothelial cells and podocytes from complement- and cytokine-mediated injury.
Cells 2021;10:1675.



87. Turco AE, Lam W, Rule AD, et al. Specific renal parenchymal-derived urinary extracellular vesicles identify age-associated structural changes in living donor kidneys.
J Extracell Vesicles 2016;5:29642.


89. Gremmels H, de Jong OG, Toorop RJ, et al. The small RNA repertoire of small extracellular vesicles isolated from donor kidney preservation fluid provides a source for biomarker discovery for organ quality and posttransplantation graft function.
Transplant Direct 2019;5:e484.



91. Gatti S, Bruno S, Deregibus MC, et al. Microvesicles derived from human adult mesenchymal stem cells protect against ischaemia-reperfusion-induced acute and chronic kidney injury.
Nephrol Dial Transplant 2011;26:1474–1483.


93. Dominguez JH, Liu Y, Gao H, Dominguez JM, Xie D, Kelly KJ. Renal tubular cell-derived extracellular vesicles accelerate the recovery of established renal ischemia reperfusion injury.
J Am Soc Nephrol 2017;28:3533–3544.



94. Cantaluppi V, Gatti S, Medica D, et al. Microvesicles derived from endothelial progenitor cells protect the kidney from ischemia-reperfusion injury by microRNA-dependent reprogramming of resident renal cells.
Kidney Int 2012;82:412–427.


95. Rastaldi MP, Armelloni S, Berra S, et al. Glomerular podocytes contain neuron-like functional synaptic vesicles.
FASEB J 2006;20:976–978.



96. Giardino L, Armelloni S, Corbelli A, et al. Podocyte glutamatergic signaling contributes to the function of the glomerular filtration barrier.
J Am Soc Nephrol 2009;20:1929–1940.



97. Li M, Corbelli A, Watanabe S, et al. Three-dimensional podocyte-endothelial cell co-cultures: assembly, validation, and application to drug testing and intercellular signaling studies.
Eur J Pharm Sci 2016;86:1–12.

















 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Supplement table 1
Supplement table 1 Print
Print















