Introduction
Acute kidney injury (AKI) is a clinical diagnosis with the characteristics of a rapidly increasing serum creatinine (sCr) level and/or decreasing urine output. The incidence of AKI is approximately 10% to 15% among non-intensive care unit hospitalizations and exceeds 50% in intensive care unit hospitalizations [
1]. AKI not only contributes to in-hospital mortality and morbidity but also increases the risk of development and progression of chronic kidney disease (CKD), major adverse cardiovascular events (MACEs), and long-term mortality [
2].
AKI and CKD are recognized as integrated/interconnected clinical syndromes. Previous studies have demonstrated CKD as a major risk factor for AKI, accounting for >30% of patients with AKI [
3]. Meanwhile, the severity and episodes of AKI could lead to CKD onset and progression [
4]; thus, AKI in CKD, also known as acute-on-chronic kidney disease (ACKD), usually results in a poor prognosis [
5].
AKI survivors are at high risk for sustained kidney injury. AKI can occur at any stage of CKD and causes renal deterioration to end-stage renal disease (ESRD). Regular evaluation and follow-up after AKI initial insult are important to improve clinical outcomes. Therefore, a standardized method to detect and diagnose AKI is necessary. In 2004, the AKI definition was first established with introduction of the Risk, Injury, Failure, Loss, and End-stage renal disease (RIFLE) protocol [
6]. The second AKI definition relies on Acute Kidney Injury Network (AKIN) criteria [
7]. Most recently, the Kidney Disease Improving Global Outcomes (KDIGO) criteria, which combined the RIFLE, AKIN, and pediatric RIFLE criteria, was modified in 2012 and is widely used for AKI definition [
8].
At present, ACKD diagnosis relies on current AKI criteria; however, the elevated sCr level in the above AKI criteria could be inadequate to diagnose ACKD, and ACKD detection could be incorrect as a result. It has been proven that even a mild increase of 25% in sCr level was associated with a 70% increase in mortality [
9]. Xu et al. [
10] set up a reference change value (RCV) of the sCr optimized criteria for AKI in CKD (cROCK) based on data from 344,694 Chinese hospitalized adults, including 27,303 CKD patients with baseline estimated glomerular filtration rate (eGFR) of Ōēż60 mL/min/1.73 m
2. The cROCK criteria are defined as a >25% increase of sCr over 7 days. Compared to the most popular KDIGO criteria, the cROCK criteria has been confirmed to improve the sensitivity in identifying patients with high risk of CKD progression in 90 days after admission, based on data from 2,383 CKD patients [
10].
Existing criteria for diagnosing AKI have remained controversial because of biological variability in CKD patients; as such, a standardized AKI definition with high prognostic ability is needed to recognize at-risk CKD patients and improve their clinical outcomes. The ACKD incidence may vary based on different diagnostic criteria. There is no report available on clinical applications of the cROCK criteria. This study aimed to evaluate the impact of the cROCK criteria in identifying ACKD and to compare the cROCK and KDIGO criteria (
Supplementary Table 1, available online) in terms of their ability to predict long-term clinical outcomes, including renal prognosis, MACEs, and all-cause mortality, in ACKD patients.
Methods
Data source and study population
We performed a single-center retrospective observational study of inpatients with CKD stage 3 at Xuzhou Central Hospital in Xuzhou, China. A total of 90,907 patients was admitted to Xuzhou Central Hospital between January 1, 2016, and June 30, 2018. Their electronic medical records (EMRs) were obtained from the hospital information system, and relevant EMR data consisted of age, sex, diagnosis code and date, sCr value, and date of admission. The eGFR was calculated using the sCr-based Chronic Kidney Disease Epidemiology Collaboration equation. Study inclusion criteria were as follows: (1) patients with CKD stage 3 (eGFR, 30ŌĆō60 mL/min/1.73 m2 for >3 months) and (2) 18ŌĆō75 years old. Exclusion criteria were as follows: (1) no sCr data available Ōēź2 times within 7 days, (2) AKI on admission, (3) underwent kidney transplantation, and (4) loss of follow-up within 3 years after discharge.
The baseline sCr value was defined as the average value of sCr within 30 days prior to admission or the first sCr value within 3 days after admission if pre-admission data were not available. According to the diagnostic criteria of KDIGO and cROCK, the patients were divided into the following four groups: KDIGO (ŌłÆ) & cROCK (ŌłÆ), KDIGO (ŌłÆ) & cROCK (+), KDIGO (+) & cROCK (ŌłÆ), and KDIGO (+) & cROCK (+). In addition, if patients met the cROCK criteria, they were defined as cROCK (+), which was the sum of KDIGO (ŌłÆ) & cROCK (+) and KDIGO (+) & cROCK (+); if they met the KDIGO criteria, they were defined as KDIGO (+), which was the sum of KDIGO (+) & cROCK (ŌłÆ) and KDIGO (+) & cROCK (+). The flowchart of study population selection and grouping is shown in
Fig. 1.
Clinical outcomes
In this study, all included patients were followed for Ōēź3 years. The primary endpoint was renal composite endpoints of CKD progression (i.e., eGFR decrease of Ōēź25%, progression to CKD stage 4, or eGFR decrease of Ōēź5 mL/min/1.73 m
2 per year), ESRD, receiving maintenance renal-replacement therapy, or death directly related to CKD [
11]. The secondary endpoints were all-cause mortality and MACEs (including cardiovascular death, myocardial infarction, and stroke).
Statistical analyses
To describe the demographic, biochemical, and clinical parameters, continuous variables are presented as mean ┬▒ standard deviation, dichotomous variables are presented as frequency and proportion, and nominal variables were analyzed with frequency distribution. The Shapiro-Wilk test was used to evaluate the normality of the variables. The differences between groups were evaluated by the Student t test for continuous variables and the chi-square test for categorical variables. The measure of inter-rater reliability was evaluated by the kappa coefficient and Fleiss kappa coefficient. Multivariate Cox proportional hazards models were performed to evaluate associations between ACKD diagnosis and renal composite endpoints, MACEs, and all-cause mortality, and results were expressed as hazard ratios (HRs) with 95% confidence interval (CIs). Harrell concordance index (C-index) was calculated to describe the predictive accuracy of clinical outcomes. Nonparametric Kaplan-Meier survival estimation was used to evaluate the effect of ACKD criteria on predicting long-term clinical outcomes, and the Kaplan-Meier survival curves were compared using the log-rank test. Receiver operator characteristic (ROC) analysis was used to assess the predictive ability of different criteria and their combinations for renal and survival outcomes. A two-sided p-value of <0.05 was defined as statistically significant. Statistical analyses were performed using the SAS version 9.4 software program (SAS Institute) and R version 4.2 software program (R Foundation for Statistical Computing).
Ethics statement
This study was retrospective. Data from the hospital information system were aggregated as secondary data without personal information, and the requirement for informed consent was waived. This study adhered to the International Conference on Harmonization guidelines for Good Clinical Practice and was conducted in accordance with the Declaration of Helsinki. The study protocol was approved by the Ethics Committee of Xuzhou Central Hospital (No. XZXY-LJ-20210110-005).
Discussion
The incidence and prevalence of CKD have increased rapidly during the past decades, and the rise in CKD burden has had a major impact on global health, resulting in increased mortality and morbidity rates worldwide [
12]. Patients with preexisting CKD have significantly higher rates of AKI compared to those without CKD, and AKI is an established risk factor for CKD development and progression [
13]. CKD progression is preventable and treatable by correcting modifiable (e.g., lifestyle, comorbidities, metabolism) risk factors [
14]. Therefore, early detection of AKI in CKD patients is crucial for these clinical applications in order to improve patient prognosis.
CKD stage 3 is the earliest stage of CKD diagnosed using sCr level, and patients with this stage of disease compose a large proportion of CKD patients. In CKD stage 3, renal function usually remains stable for a long time; however, AKI occurrence may cause rapid deterioration of renal function. Patients with CKD stages 4 to 5 were excluded from the study because it is difficult to define natural disease progression when the sCr level is increased. Therefore, our study only included adult patients with CKD stage 3.
Current AKI criteria, such as the RIFLE, AKIN, and KDIGO criteria, were developed mainly based on data from global participants without pre-existing CKD. Currently, the KDIGO criteria is one of the most widely used AKI criteria even in CKD patients in clinical practice [
8]. Few studies have focused on the AKI definition in CKD patients. The criteria for AKI are controversial because of the variability of baseline sCr level in CKD patients, which influences the RCV of sCr and AKI diagnosis. An ideal AKI definition might have the following features: 1) limited complexity, 2) diagnosis associated with short- or long-term outcomes, 3) high diagnostic accuracy with high sensitivity and specificity, and 4) relatively low cost of diagnosis [
15]. The cROCK criteria were designed based on data from a large-scale multicenter study cohort of Chinese hospitalized adult patients, and a significant proportion of these participants was adult CKD patients with initial eGFR of Ōēż60 mL/min/1.73 m
2 [
10]. Theoretically, the cROCK criteria might be more suitable than the KDIGO criteria for AKI detection in Chinese CKD patients, and the combination of cROCK and KDIGO criteria might perform even better than a single AKI criterion. However, no study has compared the effects of these criteria alone and in combination in diagnosing ACKD, such as the detection rate, the associations between ACKD and long-term clinical outcomes, and the predictive ability for long-term clinical outcomes.
The novel cROCK criteria define ACKD in CKD adults by a Ōēź25% increase in baseline sCr level over 7 days [
10], while the KDIGO criteria defines AKI by a Ōēź50% increase in baseline sCr level over 7 days. The KDIGO criteria also define AKI as an increase in the sCr level of Ōēź26.5 ┬Ąmol/L within 48 hours [
8], which requires a lower threshold; however, most patients lack repeated sCr testing results within 48 hours. Generally, the cROCK criteria should be more sensitive than the KDIGO criteria in detecting ACKD as it requires a lower threshold for an increase in sCr level (25% vs. 50%); therefore, the cROCK criteria could identify more ACKD events than the KDIGO criteria. Our results showed that the cROCK criteria detected 8.5% more ACKD events than the KDIGO criteria, indicating that the cROCK criteria were more sensitive to detecting AKI in patients with CKD stage 3.
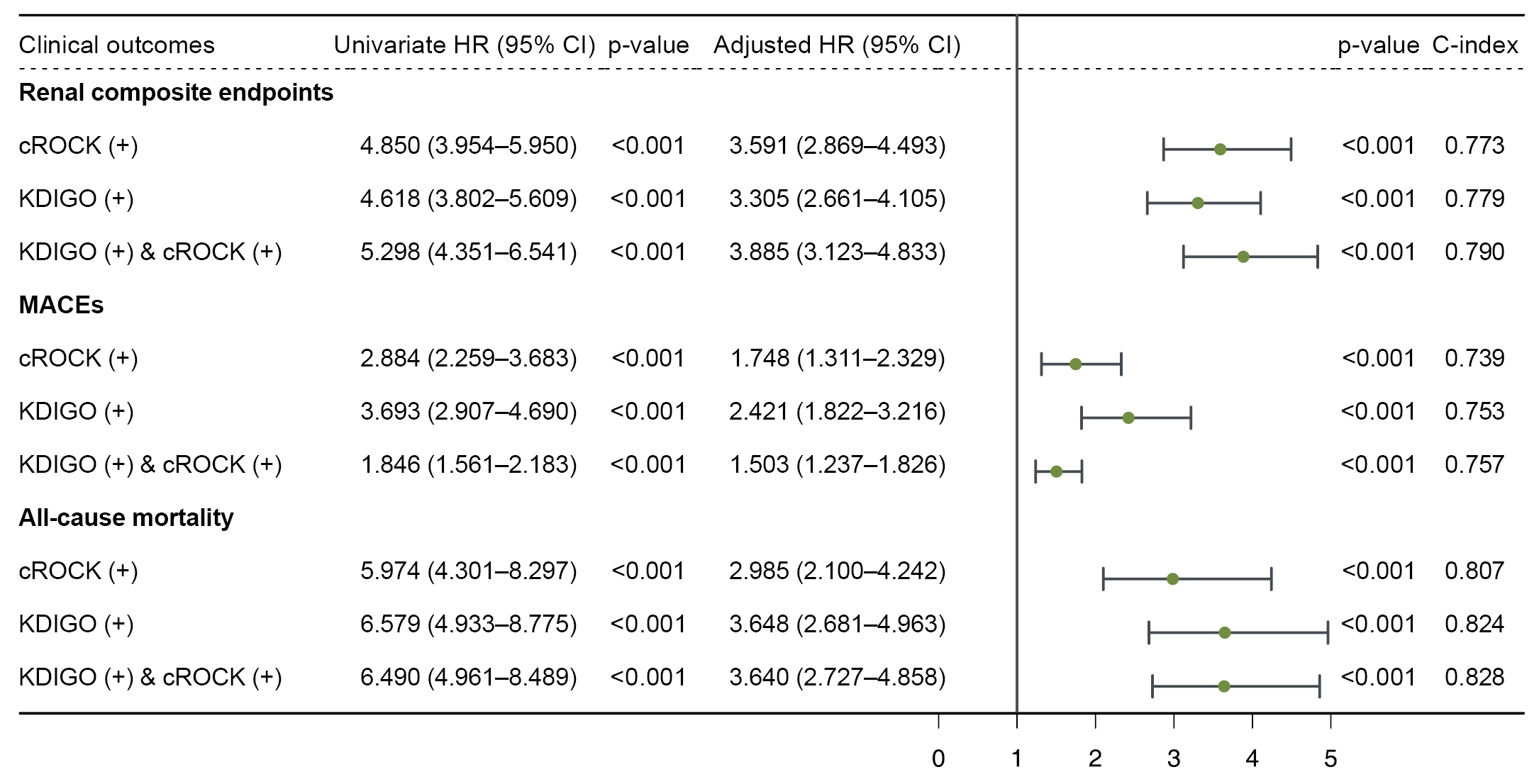
Harrell C-index is an indicator that estimates the predictive accuracy of models [
16]. A C-index value of 0.5 indicates accuracy similar to a random guess, while a C-index value of 1.0 indicates 100% predictive accuracy. In this study, during the 3-year follow-up period, all C-index values between the cROCK (+), KDIGO (+), and KDIGO (+) & cROCK (+) groups had statistically significant differences (all p < 0.05); among these, the C-index values of the KDIGO (+) & cROCK (+) group were highest for predicting renal composite endpoints, MACEs, and all-cause mortality, indicating that combining the cROCK and KDIGO criteria achieved the highest accuracy of predictive power for these three clinical outcomes.
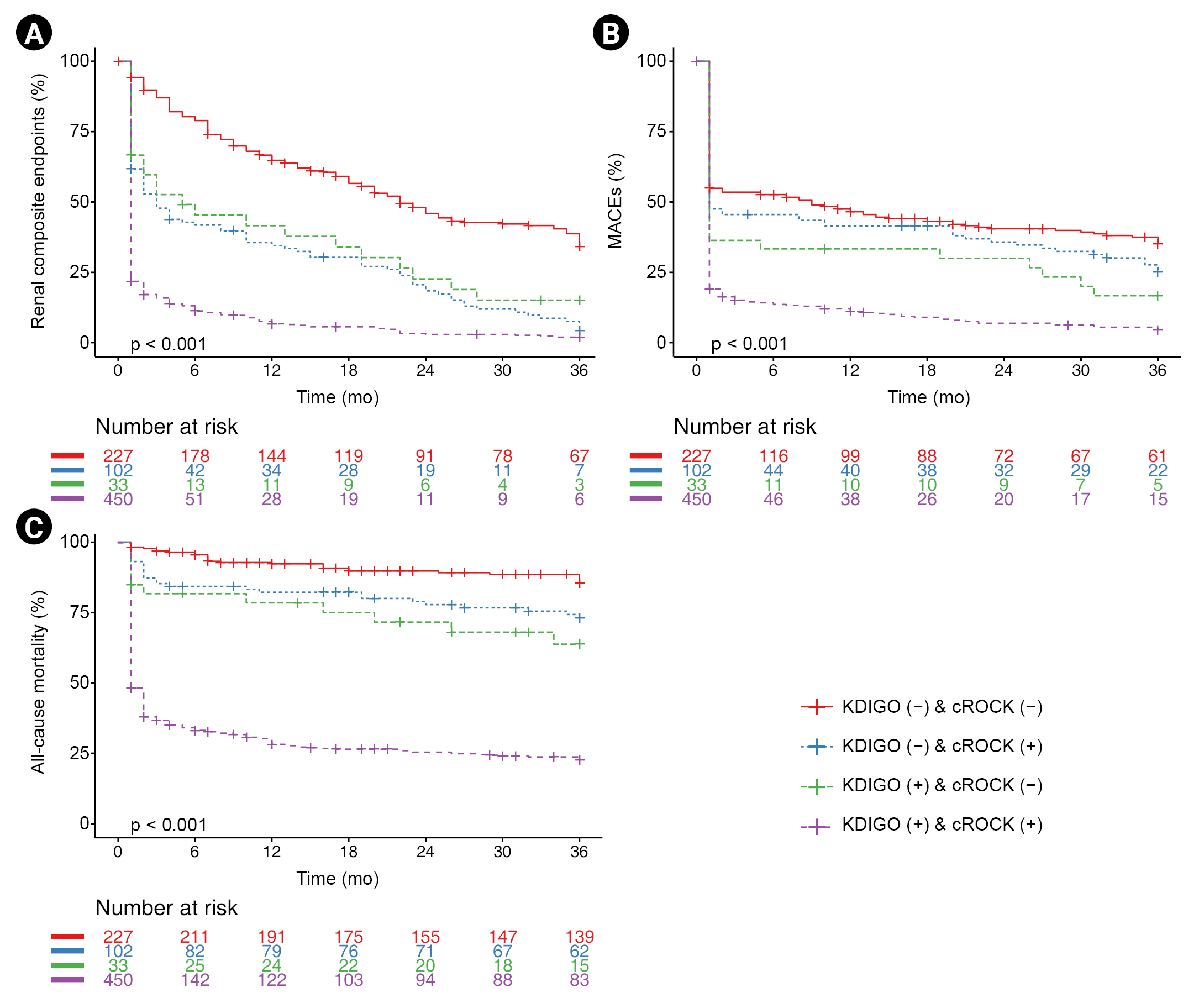
Among the four groups in
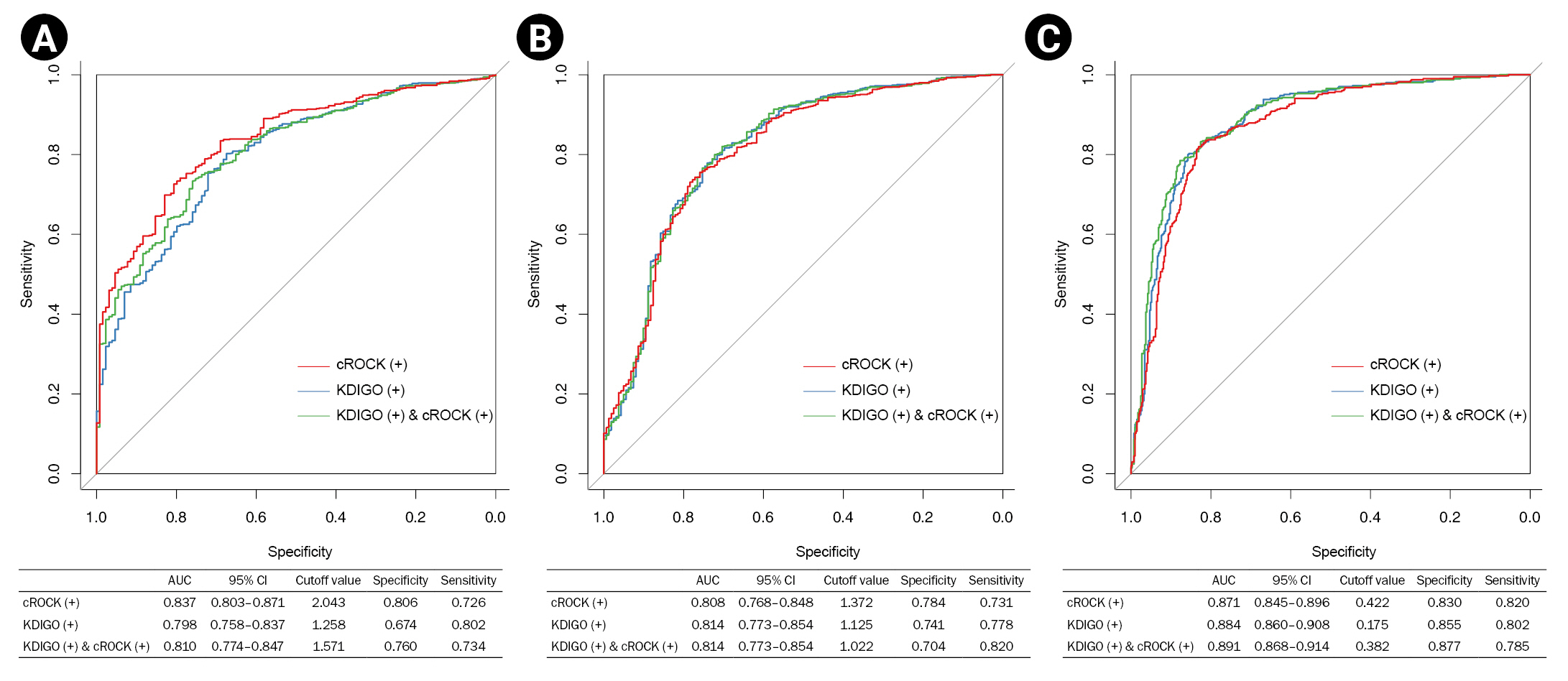
Fig. 3, ACKD diagnosed by the combined criteria of cROCK and KDIGO had the lowest survival probability of renal composite endpoints, MACEs, and all-cause mortality. Moreover, as in
Fig. 4, the cROCK criteria led to the highest AUC for predicting renal composite endpoints, and the combined criteria of cROCK and KDIGO led to the highest AUC for predicting MACEs and all-cause mortality, demonstrating that the cROCK criteria and the combination of the cROCK and KDIGO criteria had greater diagnostic accuracy with high sensitivity and specificity in predicting long-term outcomes compared to the KDIGO criteria. In addition, the cROCK criteria are defined by the RCV of sCr, and its application is simple and inexpensive. Above all, the cROCK criteria might be a reasonable AKI definition for CKD patients, and it could be applied alone or in combination with the KDIGO criteria in clinical practice.
This study has some limitations. First, this was a retrospective observational study based on an EMR dataset from a single medical center, and the performance of cROCK criteria in predicting long-term clinical outcomes in ACKD patients cannot be guaranteed in all clinical studies. Second, only 812 Chinese patients with CKD stage 3 were enrolled in the study, the heterogeneity of enrolled patients might be high, and a large proportion of patients was excluded due to incomplete data or loss of follow-up, so there might be selection bias in the study population. Third, sCr could be influenced by multiple factors, e.g., secretion from renal tubules, muscle mass, consumption of protein-containing meals, and physical activity, which might reduce its accuracy in evaluating the changes in renal function. Moreover, further studies are needed to evaluate and validate the application of the novel cROCK criteria in larger CKD populations with longer-term follow-up.
In summary, our findings demonstrated that the cROCK criteria could be applied for risk stratification of CKD patients according to ACKD status. The cROCK criteria strengthened the associations between ACKD diagnosis and long-term clinical outcomes, and the combination of the cROCK and KDIGO criteria in ACKD diagnosis might further improve the predictive ability for 3-year clinical outcomes of renal composite endpoints, MACEs, and all-cause mortality.










 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Supplement table 1
Supplement table 1 Print
Print















