Introduction
The number of hemodialysis (HD) patients increases every year and health expenditures for their treatment continue to expand [
1]. The main reasons for the recent increase in the number of HD patients are the increased prevalence of underlying comorbidities such as diabetes and hypertension as well as the increasing geriatric population [
2]. Because mortality and morbidity rates are higher in HD patients than in the general population and subsequent healthcare cost is exponentially increasing, evaluating adequacy and quality of HD service is important to improve outcomes in HD patients as well as to reduce medical cost [
3,
4].
Korea is a country with a rapidly rising prevalence of HD patients [
5], increasing nearly 50% from 42,596 in 2011 to 62,634 in 2015. Accordingly, the number of HD centers in Korea has increased by 20% from 770 in 2011 to 917 in 2015 [
6]. Therefore, an HD quality assessment tool was developed by the Health Insurance Review and Assessment (HIRA) Service to control HD quality and reduce medical costs [
7]. After a pilot survey in 2008, the HIRA has performed HD quality assessment regularly since 2009 and provided HD facilities with five-star ratings based on assessment results.
The HD facility star rating helps each HD center improve the quality of service to their patients. In addition, the rating provides useful information regarding HD facilities to the patients in a recognizable format [
8]. Many countries have their own HD quality assurance programs and star rating system for HD facilities [
3,
9ŌĆō
12]. In 2014, an international group of experts gathered to develop recommendations on how to develop and implement quality assurance measures among HD facilities [
13].
Although items included in HD quality assessment tools differ by country and are continuously amended yearly, the effects of HD quality assurance programs on patient mortality are poorly understood. Therefore, in the present study, the effects of HD facility star rating developed by the Korean HIRA on patient mortality among maintenance HD patients were evaluated.
Methods
This study was conducted in accordance with the Declaration of Helsinki. The Institutional Review Board of Ewha University Medical Center approved the study protocol (No. EUMC 2018-12-025) and written informed consent was waived due to the retrospective study design.
Study design
This was a longitudinal, observational cohort study among Korean maintenance HD patients. The baseline data including HD facility star rating were collected from HD quality assessment data starting in 2015 and mortality data collected through June 2019.
Hemodialysis facility star rating method
The HD quality assessment tool includes 12 quality measures in three domains including structural, procedural, and outcome (
Supplementary Table 1, available online). The five-star rating was determined based on the sum of weighted scores from 12 measures of HD quality (
Supplementary Table 2, available online). A total score summed up to 100. The weight was applied from 0.5 to 2.0 based on the importance of the measures. The star rating ranged from one-star to five-star based on the absolute sum of weighted scores: one-star, <65; two-star, 65 to 75; three-star, 75 to 85; four-star, 85 to 95; and five-star, Ōēź95.
Data source and study population
The target patients were 18 years of age or older who underwent HD at least twice weekly as outpatients at a single HD center during the assessment period. Subjects who were admitted to the hospital during the assessment period, received HD less than twice weekly, or transferred to another HD unit were excluded from the analysis. The HD centers selected were facilities in which HD services were performed with HD equipment and claims submitted for HD fees. The HD facilities with less than five measurements in either procedural or outcome domains were excluded from the star rating.
The HD service providers who submitted fee claims in 2015 were screened and the 12 measures in three domains (structure, process, and outcome) were assessed from October 2015 to December 2015. The assessment data were collected using a web-based data collection system. Each HD facility entered the general information regarding HD facilities, number of HD treatments, medical expenses, and number of HD equipment. In addition, information regarding the seven measures in the structural domain were entered such as personnel, availability of isolated HD equipment and emergency equipment, and satisfaction of the minimum required frequency of water quality testing. Lastly, the following patient factors in procedural and outcome domains were entered: frequency and satisfaction rate of HD adequacy, vascular access stenosis monitoring, frequency of regular laboratory tests, and satisfaction rate of calcium and phosphorus control. Data retrieved from the web-based database were compared with the data from electronic medical records to confirm the accuracy and reliability.
Sociodemographic and clinical data were obtained from the HIRA database. The sociodemographic factors collected included age, sex, dialysis vintage, cause of end-stage renal disease, body mass index, and health insurance status. The medical comorbidities of the subjects were identified by reviewing the medical history 1 year before the initiation of dialysis therapy. The International Classification of Disease (ICD-10) codes were used to extract the following comorbidities: ischemic heart disease (I20ŌĆō25), congestive heart failure (I50), cerebrovascular disease (I60ŌĆō64, I69), diabetes mellitus (E10ŌĆō14), hypertension (I10ŌĆō13, I15), and atrial fibrillation (I48). Predialysis systolic and diastolic blood pressures were measured. The laboratory parameters including plasma hemoglobin, serum albumin, calcium, and phosphorus, were collected every month during the assessment period. The single-pool Kt/V was measured as an indicator of HD adequacy. The date of the patientŌĆÖs death was estimated from the date of insurance loss.
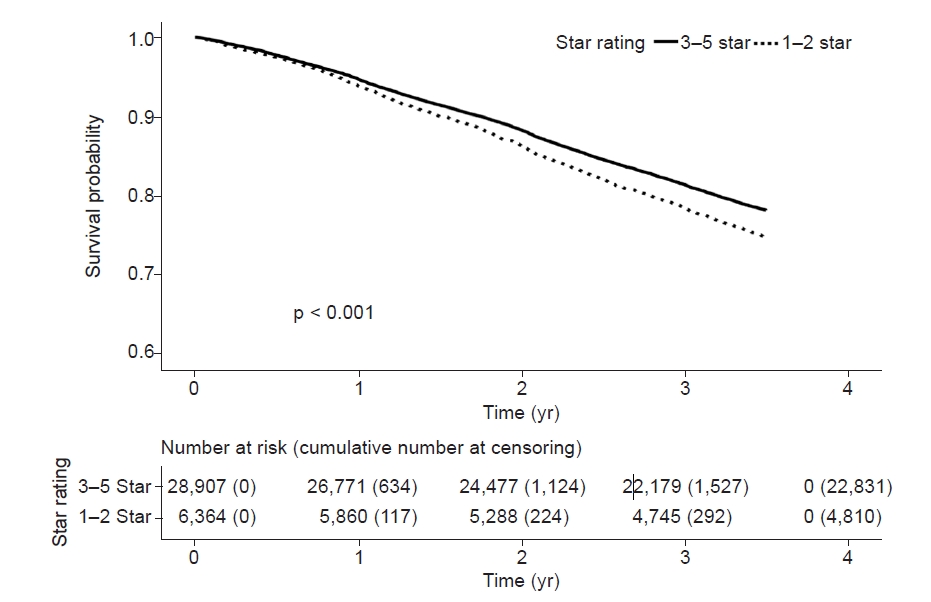
Statistical analyses
Statistical analyses were performed using SAS Enterprise Guide 6.1 (SAS Institute). The subjects were divided into two groups based on star rating: low star rating (one or two stars) and high star rating (three to five stars). The chi-square test was used to compare categorical variables and independent t test was used to compare continuous variables between groups. Kaplan-Meier survival curves were used to compare the risk of mortality between groups. The patients who received kidney transplantation after HD quality assessment were censored in survival analysis. Multivariable-adjusted Cox proportional hazards model was used to evaluate star rating as an independent variable for mortality. Model 1 was adjusted for age, sex, dialysis vintage, and body mass index. Model 2 was adjusted for medical comorbidities in addition to the factors included in model 1. Model 3 was adjusted for all sociodemographic and clinical factors including health insurance status and laboratory parameters. Finally, subgroup analyses were used to define the relative risk of mortality based on star rating.
Discussion
In this prospective cohort study using nationwide HD quality assessment data, the effects of HD facility star rating on patient mortality were evaluated. The patients in the HD facilities with low star ratings (one or two stars) showed lower HD adequacy, higher serum calcium and phosphorus levels as well as higher diastolic blood pressure. The HD facilities with low star ratings had poorer patient survival compared with high-star-rating facilities. Multivariable Cox regression analysis showed that low HD facility star rating increased patient mortality risk by approximately 11%.
In the United States, the Centers for Medicare and Medicaid Services launched the end-stage renal disease Quality Incentive Program (QIP) in 2012 to pay for performance based on quality improvement [
14]. In addition, the Centers for Medicare and Medicaid Services launched the Dialysis Facility Compare Star Program in 2015 with the purpose of presenting differences in quality of care among dialysis facilities based on the reported quality measures [
12]. Since then, the distribution of HD facility star rating has shifted upward showing an improvement in quality of HD care [
8]. The QIP and Dialysis Facility Compare Star Program is similar to the Korean HD quality assessment and HD facility five-star rating systems. Although the HD quality assessment tool and HD facility star rating system were developed to improve patient health outcome, minimal research has been conducted regarding their effect on patient outcome. In addition, discussing the effects of the QIP program or star rating system on patient outcome has been difficult because many indicators of quality assessment have changed over time and each version has not yet been compared.
This is the first study in which the effects of HD quality assessment and HD facility star rating system on patient mortality among prevalent HD patients were reported. Recently, Ajmal et al. [
15] reported the dialysis facilities with low QIP scores were associated with a higher mortality rate within 1 year of beginning HD among incident patients. However, the effects of HD facility star rating system on long-term patient mortality have not been investigated in any other study. We prospectively collected survival data during a mean follow-up of 3 years. The results showed HD facility star rating is also independently associated with long-term patient mortality.
Significant attention has been given to patient characteristics to improve clinical outcome among HD patients. Patient characteristics such as age, presence of diabetes mellitus, previous cardiovascular disease, and low level of serum albumin are associated with higher mortality risk in HD patients [
16]. In addition, increasing HD efficacy and treating anemia and mineral bone disorders may be important for improving patient outcome. However, increasing HD dose/frequency in previous large-scale clinical trials failed to reduce all-cause mortality [
17ŌĆō
19] or manage anemia [
20] and mineral bone disease [
21]. Conversely, minimal attention has been given to the effects of structural and procedural components of HD service on patient outcome. In a recent study by Ajmal et al. [
15], the clinical effects of QIP measures on patient outcome were evaluated. The United States QIP data includes percentage of waste removed during HD (HD adequacy), percentage of anemia overcorrection (plasma hemoglobin > 12.0 g/dL), vascular access type, infection rate, In-Center HD Consumer Assessment of Healthcare Providers and Systems, monthly reporting of calcium and phosphorus levels, monthly dosage of erythropoietin-stimulating agents, and monthly reporting of hemoglobin and hematocrit levels [
12]. However, QIP has been criticized for including easily obtained laboratory measures with a limited evaluation regarding patient outcome [
22ŌĆō
24]. To improve the quality of HD care, decreasing the workload of HD personnel, improving the water treatment process, reducing events associated with vascular access, and regularly monitoring patient-related outcomes are essential. The strength of the Korean HD facility star rating system is the inclusion of structural and procedural indicators. For example, evaluating the percentage of vascular access (catheter vs. fistula) and the satisfaction rate of regular monitoring for the stenosis of arteriovenous fistula is part of the system. In addition, physician-to-patient ratio and proportion of experienced personnel in each HD unit are monitored. In a recent study by Harley et al. [
25], high nephrology caseload was reportedly associated with poor patient outcome. Therefore, structural components in addition to laboratory measures may affect patient mortality.
In the present study, patients from low-star-rating HD facilities had more comorbidities and poorer clinical indices such as higher blood pressure and lower hemoglobin and albumin levels. However, whether this is due to the large portion of elderly patients or poor patient management in low-star-rating HD facilities is unclear. However, HD facility star rating remained an independent risk factor for patient mortality after adjusting for known risk factors including older age, male sex, medical comorbidities, and health insurance status.
The present study had several limitations. Because this study was from a single country with data from a single assessment year, the results may not be generalized. The baseline covariates between two HD facility star rating groups were not balanced before analysis using propensity score matching. Each component of star rating was not analyzed, therefore, which component of HD quality assessment mainly affected patient mortality could not be determined. In addition, the cause of death was not analyzed. In addition, disease-specific mortality was not compared between groups. Further studies should be performed to evaluate the importance of each indicator (facility personnel or procedural indicator) or underlying disease for all-cause mortality and specific patient outcomes. Patients admitted to the hospital were excluded from the analysis, therefore, patients with severe comorbidities or those admitted to nursing hospitals may have been excluded from the analysis. Next, this study was performed with only prevalent HD patients. Therefore, the effect of HD quality assessment on incident HD patients cannot be determined from this study. In addition, whether the current HD facility star rating scoring system is optimal is beyond the scope of this study. Further studies are needed to validate the current scoring system and determine whether the star rating system is optimal. Lastly, whether star rating of HD facilities improves patient outcome cannot be concluded from the results and may be deduced in another study with sequential HD quality assessment data.
In conclusion, the low HD facility star rating based on HD quality assessment may result in higher patient mortality. Further prospective studies are needed to prove whether improvement in star rating reduces patient mortality.
















 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Supplement table 1
Supplement table 1 Print
Print















