Kidney Health Plan 2033 in Korea: bridging the gap between the present and the future
Article information
Abstract
In response to the increase in the prevalence of chronic kidney disease (CKD) in Korea, the growth of patients requiring renal replacement therapy and the subsequent increase in medical costs, the rapid expansion of patients with end-stage kidney disease (ESKD), and the decrease in patients receiving home therapy, including peritoneal dialysis, the Korean Society of Nephrology has proclaimed the new policy, Kidney Health Plan 2033 (KHP 2033). KHP 2033 would serve as a milestone to bridge the current issues to a future solution by directing the prevention and progression of CKD and ESKD, particularly diabetic kidney disease, and increasing the proportion of home therapy, thereby reducing the socioeconomic burden of kidney disease and improving the quality of life. Here, we provide the background for the necessity of KHP 2033, as well as the contents of KHP 2033, and enlighten the Korean Society of Nephrology’s future goals. Together with patients, healthcare providers, academic societies, and national policymakers, we need to move forward with goal-oriented drive and leadership to achieve these goals.
Introduction
Chronic kidney disease (CKD) is a major public health issue that causes early death and poor quality of life. The global prevalence of CKD is approximately 10%; however, it varies by region, country, and study design, reaching up to 13.4% in systematic reviews and meta-analyses [1–3]. Furthermore, CKD has emerged as a leading cause of mortality, accounting for 1.2 million deaths globally. As a cause of death, it has ranked from being the 19th leading cause in 2013 to the 12th in 2017 and is expected to rank 5th in 2040 [3]. Aside from mortality, disease burden is an essential value in determining health policy. The burden of CKD is increasing in all aspects of disease burden, including incidence, prevalence, mortality, and disability-adjusted life years, particularly serious in low- and lower-middle-income countries [4–6].
As diabetes mellitus (DM) and hypertension are the leading causes of CKD in most areas of the world, CKD prevalence is expected to increase with the growing incidence of DM and increase in the elderly population. The current state of CKD in Korea is comparable with the global status of CKD. The Korean National Health and Nutrition Examination Survey (KNHANES) data shows that the prevalence of CKD (estimated glomerular filtration rate [eGFR] of <60 mL/min/1.73 m2 and/or albuminuria) among adults aged >18 years in 2012 was 8.0%, which has increased to 8.4% by 2021 [7]. Moreover, based on the data from the United States Renal Data System (USRDS), the incidence of treated end-stage kidney disease (ESKD) in Korea (355 per million population [PMP] in 2020) was the fourth highest globally, and Korea (9.7 PMP) had the largest average yearly increases in the incidence of treated ESKD attributed to DM between 2010 and 2020 worldwide [8].
In response to the high ESKD incidence, particularly diabetic kidney disease (DKD), the disproportional expansion of hemodialysis (HD) patients, and the resulting increase in medical costs in Korea to date, the Korean Society of Nephrology (KSN) recently suggested the “Kidney Health Plan 2033 (KHP 2033)” for national kidney health. KHP 2033 established the objective of “leading a healthy society through improvement of public kidney health” and provided a vision of “active prevention, treatment, and management of CKD,” “reduction of socioeconomic burden,” and “increased quality of patient-centered treatment.”
In this special article, we first discuss the current state of CKD and ESKD in Korea, focusing on DKD prevalence and medical costs. Moreover, we provide current statistics on home therapy in Korea, including peritoneal dialysis (PD) and kidney transplants. Lastly, we suggest missions and action plans for KHP 2033 as a milestone to bridge the gap between the present and the future.
The current challenges in kidney health in Korea
Increasing chronic kidney disease and end-stage kidney disease prevalence
As stated in the KSN fact sheet, it is estimated that one in every nine adults in Korea has CKD, with a total patient population of around 4.6 million [9]. CKD has an extremely high severity that patients with CKD have a 7.2-fold higher risk of death than normal individuals. According to the data of the National Health Insurance Service and the Health Insurance Review and Assessment Service (HIRA), CKD was the disease with the highest medical cost per patient. In 2021, 8,369,000 Korean won (KRW; 7,692 US dollars) was spent for the treatment of one patient, which was more than twice the amount of 3,719,000 KRW (3,418 US dollars) for malignant disease, which ranks second in terms of medical cost per patient. As CKD progressed, the cost of treatment per person increased. Compared with a patient with hypertension, the cost was 3-, 5-, and 21-fold higher in patients with stages 3, 4, and 5 predialysis CKD, respectively. In 2021, the total cost of reimbursement on CKD was over 2.3 trillion KRW (2.08 billion US dollars) in Korea.
As reported by the 2022 Korean Renal Data System (KORDS) of the KSN, the number of patients with ESKD receiving renal replacement therapy (RRT) in Korea reached 127,068 (Fig. 1) [10]. Among them, 78% were receiving HD, and 3.0 trillion KRW (2.71 billion US dollars) was spent on dialysis treatment annually [11].

The number of patients with renal replacement therapy in Korea from the 2022 Korean Renal Data System report of the Korean Society of Nephrology.
ESKD, end-stage kidney disease.
Compared with other countries, the increasing trend of CKD in Korea is serious. According to the 2022 Annual Report of the USRDS, comparing 2010 and 2020, the average annual increase in ESKD incidence was 18.8 PMP, the second highest in the world following Thailand (Fig. 2A). Particularly, the average annual increase in the number of patients with ESKD due to DM was 9.7 PMP, the highest among all countries surveyed. Among countries or regions with the highest percentage increase in 2019–2020 vs. that in 2010–2011, the prevalence of ESKD treated in Korea more than doubled over this period (2010 vs. 2020) (Fig. 2B) [8].
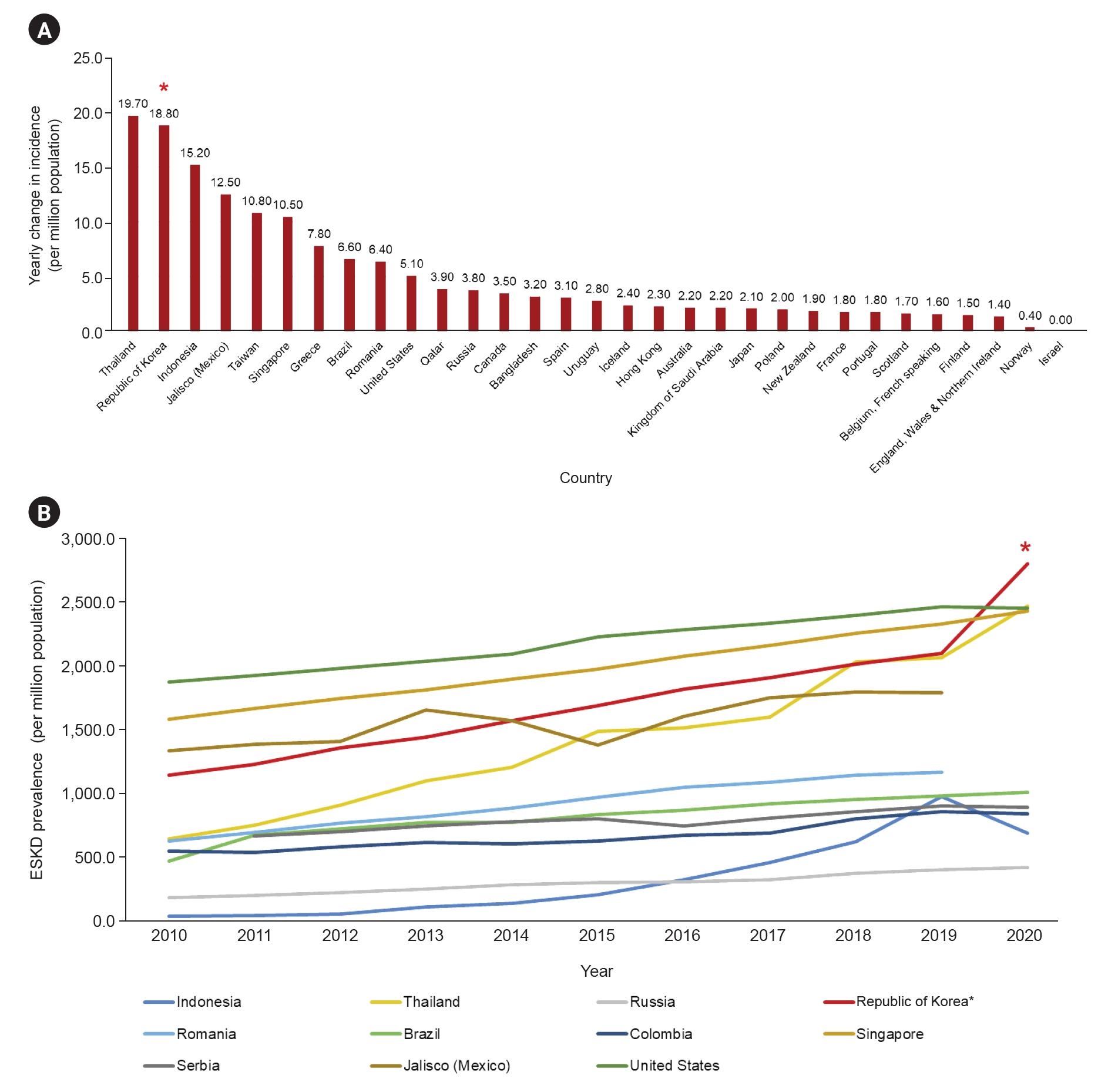
Prevalence of treated ESKD in countries or regions with the largest percentage increase in prevalence, 2010 vs. 2020 (data from 2022 USRDS annual data report).
(A) Average yearly change in the incidence of treated ESKD by country or region, 2010 vs. 2020. (B) Prevalence of treated ESKD in countries or regions with the largest percentage increase in prevalence, 2010 vs. 2020.
ESKD, end-stage kidney disease.
Data sources: https://usrds-adr.niddk.nih.gov/2022/end-stage-renal-disease/11-international-comparisons
Diabetic kidney diseases: a lethal and progressive burden to the Korean society
In Korea, as DKD was the main cause of ESKD, we focused on the current status of DKD and ESKD epidemics. Furthermore, we analyzed the medical cost of HD patients depending on diabetic status based on HIRA data.
Diabetic kidney disease epidemiology in Korea: from big data
A study reported the DKD prevalence in Korea by analyzing the KNHANES V conducted in 2011 [12]. In this study, albuminuria was defined as >30 mg/g and CKD was defined as an eGFR of <60 mL/min/1.73 m2. Among participants with DM, 26.7% and 8.6% had albuminuria and CKD, respectively. DM increased the risk of albuminuria and CKD by 2.5 and 1.8 times, respectively [12]. The age-standardized rate of DKD prevalence in 2015 was 12,400 per 100,000 individuals in patients with DM, 12,900 per 100,000 in males and 11,800 per 100,000 in females. In patients with DM aged ≥ 30 years, DKD prevalence increased from 8.4% to 12.4% between 2006 and 2015 [13]. Additionally, the incidence of ESKD among the diabetic population was 13.8-fold higher than that among the nondiabetic population [13]. In this study, as of 2015, the standardized incidence rates (per 100,000) of ESKD in diabetic and nondiabetic individuals were 109.0 and 7.9, and the standardized prevalence rates (per 100,000) were 860.8 and 39.3, respectively. Furthermore, DM is associated with a poor prognosis in patients with CKD. In a study with the KNOW-CKD cohort, patients with DM had higher risks of renal function deterioration, ESKD, cardiovascular complications, and death than those without DM [14].
The comparison of USRDS international data revealed that the incidence of ESKD due to DM was 177 PMP in 2020, the fourth highest among 45 countries and the third highest among 12 Asian countries. Between 2010 and 2020, the average annual increase in the incidence of diabetic ESKD was 9.7 PMP, which was the highest among 37 countries. Compared with 2010, the overall ESKD incidence percentage increased by 96.2% in 2020, showing a high correlation with the 84.6% increase in ESKD incidence due to DM. This suggests that DM has recently led to an increase in patients with ESKD in Korea [8].
Status of diabetic end-stage kidney disease: data from the Korean Renal Data System
As in other countries, DM is the most significant cause of ESKD in Korea. According to KORDS data, it has maintained the highest ranking since 1994 and accounted for 47.8% of the causes of ESKD in 2022 [10]. DM was followed by hypertension and glomerulonephritis, with percentages of 21.5% and 9.4%, respectively.
The trends observed in the epidemiologic characteristics of diabetic ESKD in Korea after analyzing the 2021 KORDS data (unpublished data) revealed that the proportion of diabetic and nondiabetic ESKD was 50.3% and 49.7%, respectively, in HD patients, whereas they were 45.5% and 54.5%, respectively, in PD patients. The trend for all-cause mortality showed a gradual decrease since 2001. The decreasing trend of mortality is similar in both HD and PD patients. In the analysis of the cause of death, cardiac origin was 38.4% in patients with diabetic ESKD, which was higher than 30.3% in patients with nondiabetic ESKD. Patients with diabetic ESKD had more comorbidities, including cardiac disease, vascular disease, and pneumonia, than those with nondiabetic ESKD (unpublished data).
Burden to the Korean society: an analysis from Health Insurance Review and Assessment Service data
1) Data source
To gather demographic and clinical data of individual HD patients, we used HD quality assessment data and HIRA claims data collected from October to December 2015. This analysis was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (IRB) of Hallym University Kangnam Sacred Heart Hospital (No. HKS 2021-11-043). The IRB waived the need for written informed consent from the patients because the identity of study participants was unknown in this study. Adult HD patients aged ≥18 years who received HD treatment ≥2 times weekly as outpatients were included in this assessment. Patients who were admitted during assessment or lost to follow up were excluded from the analysis [15]. Additionally, the HD quality assessment collected data from each HD facility through a web-based data-collection system [16,17].
The total costs of medical treatments were the sum of the reimbursed expenses, the data for which was extracted from the HIRA claims data between January 2016 and November 2021. Claims data generated at the hospital included the costs of the medical examination, medication, counseling, laboratory tests, procedures, and surgeries that may have been prescribed by the doctor. The total costs of medical treatments included the claim data for total visits to outpatient clinics and hospitalization [18]. We calculated the amounts paid by the provider and the individual patient per year to determine the total medical cost per person per year. In addition, the annual provider’s payment and patient’s payment were calculated, respectively, and the annual outpatient cost and cost of hospitalization were calculated. The exchange rate to US dollar presented in this study was the rate in 2019.
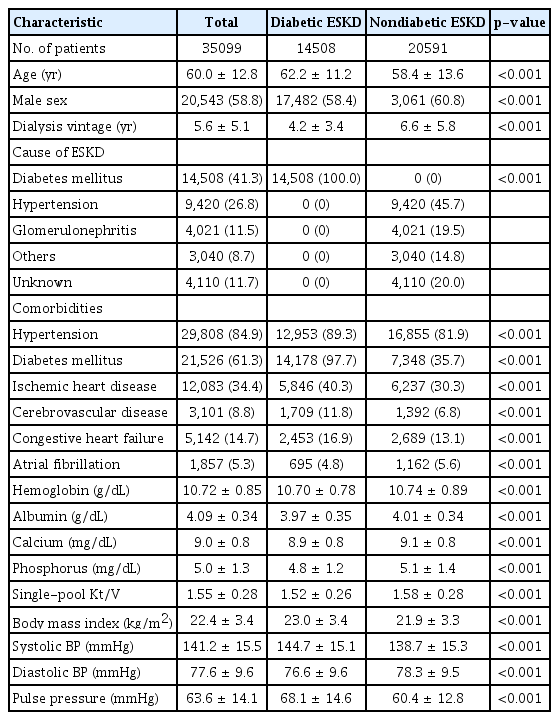
2) Characteristics of patients with diabetic end-stage kidney disease in Korea
Among the patients, the mean age of the diabetic ESKD group was 60.0 ± 12.8 years, and male participants comprised 58.4%, which was smaller than that of the nondiabetic ESKD group. Dialysis vintage was 4.2 ± 3.4 years in patients with diabetic ESKD, which was shorter than 6.6 ± 5.8 years in patients with nondiabetic ESKD. In the nondiabetic ESKD group, the causes of ESKD were hypertension (45.7%), unknown etiology (20.0%), and glomerulonephritis (19.5%). Patients with diabetic ESKD had lower serum levels of hemoglobin, albumin, calcium, phosphorus, and spKt/V than those with nondiabetic ESKD. Patients with diabetic ESKD had higher systolic blood pressure and pulse pressure than those with nondiabetic ESKD (Table 1).
3) Trend of using medical facilities in diabetic and nondiabetic end-stage kidney disease
In terms of medical insurance, Medical Aid was used for 20.9% of patients with diabetic ESKD and 24.3% of patients with nondiabetic ESKD. Medical Aid is a type of social security system in which the government provides medical care for low-income citizens who cannot maintain their livelihood or have difficulty making a living [19]. The number of patients with diabetic ESKD receiving dialysis treatment at general or tertiary hospitals was higher than that of patients with nondiabetic ESKD.
In all patients, the annual number of outpatient clinic visits was 119.7 ± 60.8 visits per year, and the annual number of emergency department visits was 0.8 ± 1.3 visits per year. The annual number of hospitalizations was 2.5 ± 3.4 times, and the mean duration of hospitalization was 28.0 ± 55.1 days. Diabetic ESKD had more annual outpatient clinic visits (124.5 ± 59.7 visits/yr vs. 116.3 ± 61.4 visits/yr, p < 0.001) and annual emergency department visits (1.0 ± 1.5 visits/yr vs. 0.6 ± 1.1 visits/yr, p < 0.001) than nondiabetic ESKD. The annual number of hospitalizations was 3.2 ± 3.9 visits per year, which was higher than that of patients with nondiabetic ESKD (p < 0.001); the mean duration of hospitalization was longer (37.1 ± 63.1 days vs. 21.5 ± 47.7 days, p < 0.001) than that of patients with nondiabetic ESKD.
4) Comparison of medical costs in diabetic and nondiabetic end-stage kidney disease
Patients with diabetic ESKD had higher annual total medical costs than those with nondiabetic ESKD (p < 0.001). Furthermore, the annual cost of patient’s and provider’s payments was higher in patients with diabetic ESKD than in those with nondiabetic ESKD (p < 0.001). Additionally, medical costs due to hospitalizations and visits to outpatient clinics were higher in patients with diabetic ESKD (p < 0.001) (Fig. 3). However, no difference in medication cost was observed between the two groups (p = 0.67).
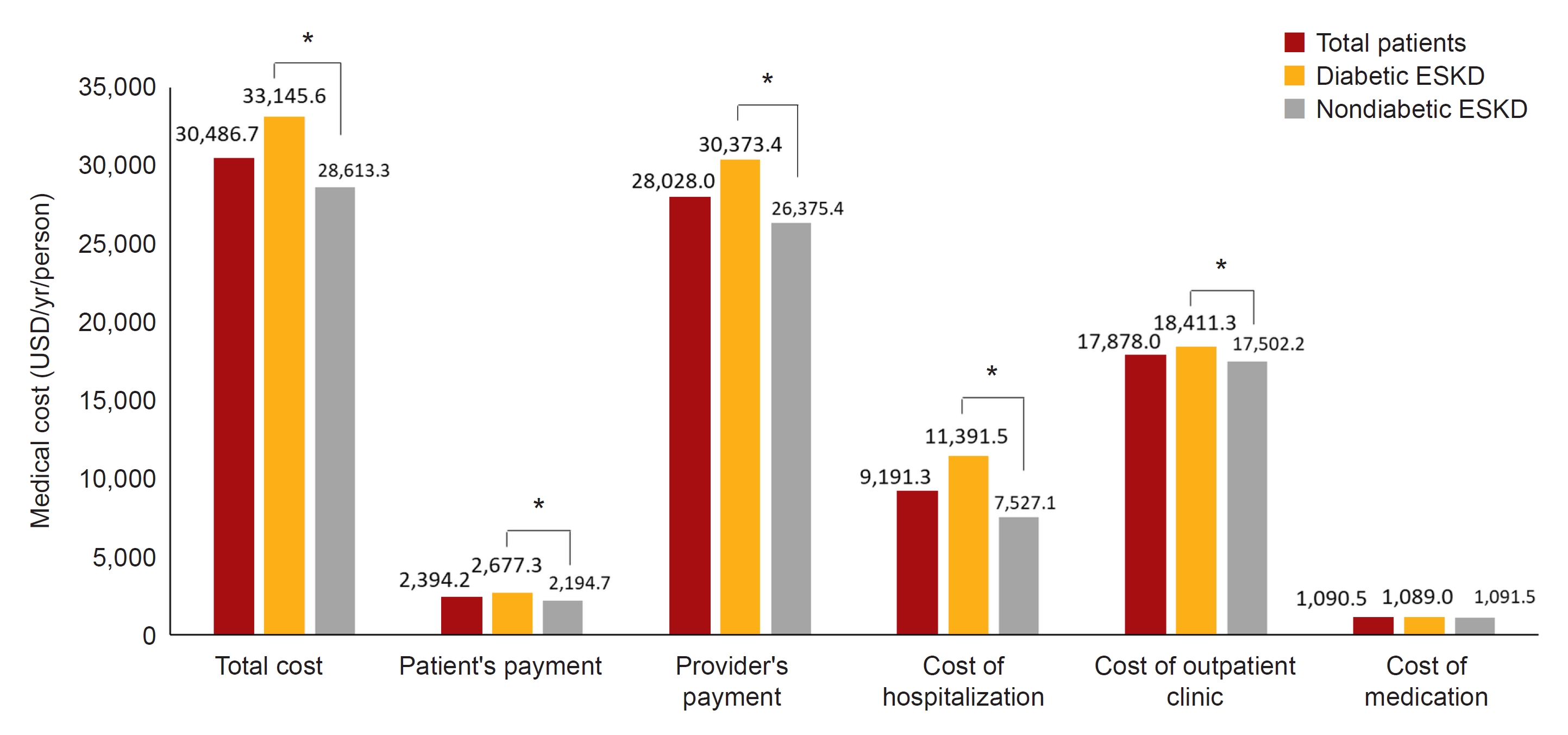
Medical cost of patients with diabetic and nondiabetic ESKD (US dollars/person/yr).
Patients with diabetic ESKD had higher annual total medical costs than those with nondiabetic ESKD, and the annual cost of patient’s and provider’s payments was higher in patients with diabetic ESKD than in those with nondiabetic ESKD. In addition, medical costs due to hospitalizations and visits to outpatient clinics were higher in patients with diabetic ESKD.
ESKD, end-stage kidney disease. *p < 0.001.
Home therapy: challenges and future directions in Korea
When CKD progresses and patients exhibit uremic symptoms, they are recommended to undergo RRT such as kidney transplantation, HD, and PD. Kidney transplantation is the most ideal type of RRT with the highest survival rate and the lowest cost in the long term. However, most patients undergo dialysis due to the lack of donors. Unlike HD patients, stable kidney transplant patients do not need to visit the hospital frequently, so kidney transplantation is a type of home therapy.
PD, another type of home RRT, requires fewer hospital visits and is more flexible than HD. Therefore, PD facilitates social activities, including working and studying, and is advantageous for the maintenance of patients’ independence and economic activities [20]. Furthermore, as the risk of hypotension or arrhythmia is low, and residual renal function is maintained longer than HD, PD is possible in small children or patients with poor vascular access [21]. These characteristics of PD might help improve patients’ quality of life [22].
Recently, in several domestic and international studies, the mortality rate of dialysis patients has been improved, particularly in PD; accordingly, the mortality rate of PD is lower than that of HD. In Korea, the mortality rate of PD has been lower than that of HD since 2019; this pattern has also been observed in countries, such as the United States and Australia [8,10,23,24]. Moreover, it is suggested as a pretransplant modality because patients with PD had better post-transplant outcomes than those with HD before transplantation [25,26].
Several studies have reported the effect of PD on the reduction of socioeconomic burden [20,27]. In one study, the authors analyzed the annual medical costs of dialysis patients in Korea in 2017. In this study, HD costs 22 million KRW/person (20,236 US dollars/person), which is 1.36-fold higher than that of PD, which costs approximately 16 million KRW/person (14,717 US dollars/person) [28]. The mortality rate of PD patients decreased; therefore, the socioeconomic burden from high mortality is also reduced. Furthermore, nonmedical costs, including transportation, dialysis machines, water purification, electricity, and patient time lost, are also reduced [29,30]. As patients can maintain their jobs during treatment, economic losses are further reduced [31]. In addition, PD patients had lesser psychological distress than HD patients during the COVID-19 pandemic when social distancing was required [32].
However, despite these advantages of PD, the number of patients with PD is decreasing compared to HD or kidney transplants. The PD rate among patients with ESKD is continuously decreasing from 28% in 2006 to 4.4% in 2021 [10]. There is a small number of patients who cannot receive PD, and a study has shown that approximately 78% of patients with ESKD can be considered for PD [33,34]. However, for various reasons, 83.6% of patients who started RRT in 2021 selected HD.
In Korea, several factors contribute to the reduced PD uptake in patients with ESKD, including healthcare policy or lack of incentives for PD, growing numbers of for-profit HD units, lack of manpower (particularly nurses) dedicated to PD, and lack of appropriate process for dialysis modality selection (shared decision-making). To expand home therapy in Korea, several aspects, including national government support, the development of technology, and educational programs for individual patients, should be considered.
The mission for the future: the Kidney Health Plan 2033
Recognizing the situation in Korea, the KSN proposed the KHP 2033 and has set three action goals for reducing the socioeconomic burden of dialysis and improving the quality of patient-centered treatment by preventing ESKD occurrence and increasing the home therapy rate. The three action goals to be achieved by 2033 are as follows: 1) a 10% reduction in the number of patients with CKD, 2) a 10% decrease in the proportion of patients with DKD in ESKD, and 3) an increase up to 33% of home therapy (PD + transplant) proportion in patients with ESKD. Each goal needs to be determined and then evaluated using the method described above. CKD prevalence reflects the proportion of patients with eGFR of <60 mL/min/1.73 m2 or albuminuria among all patients included in the KNHANES. The second and third goals can be compared based on KORDS data.
What are the action plans of Kidney Health Plan 2033?
KSN set up four major areas, including patients, practice, partner, and policy (4Ps), for the effective achievement of the three action goals, and subsequently established action plans for each area. The overview of KHP 2033, including each action plan, is summarized in Fig. 4. For the development and implementation of detailed action plans, KSN cooperated with its committees, including the KORDS registry, the Clinical Practice Guidelines, the Collaborative Studies, and the Public Relation.
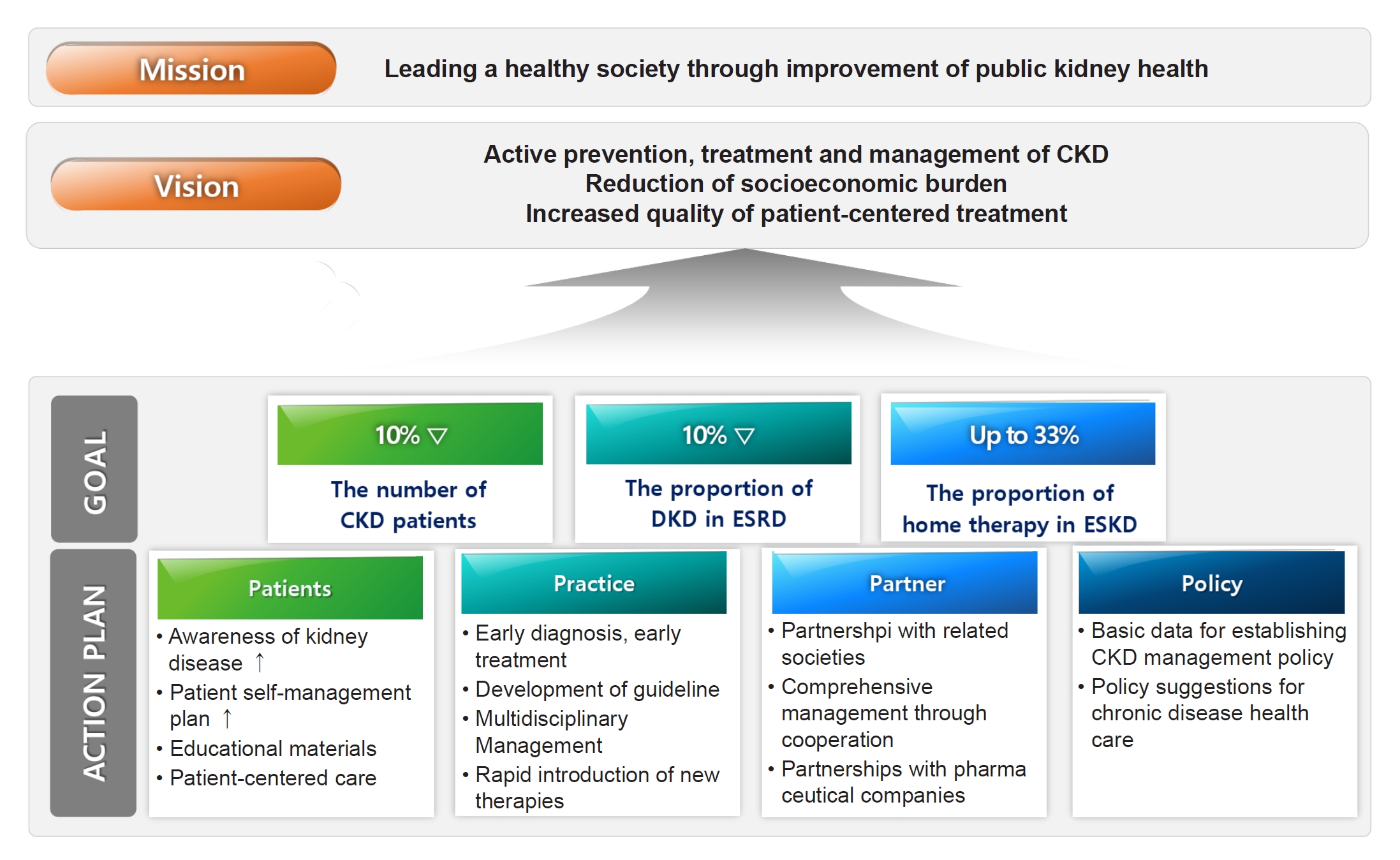
Kidney Health Plan 2033 overview.
The Korean Society of Nephrology set three goals and four action plans to achieve those goals.
CKD, chronic kidney disease; DKD, diabetic kidney disease; ESKD, end-stage kidney disease; ESRD, end-stage renal disease.
KHP 2033 attempts to accurately grasp the current situation in Korea through different data sources. We identified and summarized domestic and foreign references related to CKD, ESKD, and DKD prevalence or incidence in Korea. We analyzed KORDS data to identify the status of ESKD and home therapy more specifically as well as examined costs related to dialysis in connection with the National Health Insurance Service (NHIS). Moreover, KSN conducted research on DKD using big data from national health insurance with the Korean Diabetic Kidney Disease Working Group, an affiliated organization, and supported the establishment of a DKD cohort. Accumulated data from KHP 2033 will be valuable basic information for patient education and policy proposals.
A significant achievement regarding clinical practice is the development of Korean DKD treatment guidelines [35]. This guideline reflects Korea’s special circumstances, including DKD epidemiology and reimbursement regulation by the NHIS. Particularly, this guideline recommends consultation with a nephrologist from the early stage of DKD (moderately increased albuminuria or eGFR below 60 mL/min/1.73 m2), emphasizing active and early intervention for DKD prevention.
KSN participates in and supports the “Pilot Project for Home Management of PD Patients” by the Ministry of Health and Welfare. Patients can receive professional educational counseling for dialysis management and receive close monitoring by medical staff through the pilot project. In the analysis of registered patients from 11 institutions, peritonitis and dialysis-related complications decreased following the pilot project implementation. Additionally, monitored patients had lower hospitalizations, emergency department visits, mortality, and medical costs than non-registered patients in the pilot project (unpublished results).
To improve public awareness of kidney disease, KSN continues to promote KHP 2033 through YouTube, newsletters, symposiums, and press conferences. Moreover, KHP 2033 plans to continue policy proposal activities, including policy forums and expert roundtables, to generate health policies that are impactful to the public.
The action plans and the progress of KHP 2033 toward each action goal are summarized in Table 2.
In summary, we focus on the following three significant aspects of kidney health problems in Korea: 1) the rapid increase in CKD and ESKD populations; 2) the constantly increasing diabetic ESKD incidence and increase in medical costs associated with the aforementioned two factors; and 3) the decrease in the number of patients treated with home therapy, particularly PD. To address the current situation, we established the following three main goals: 1) a 10% decrease in the number of patients with CKD; 2) a 10% decrease in the proportion of patients with DKD in new patients receiving RRT; and 3) an increase of up to 33% in the proportion of patients with ESKD treated with home therapy, including PD and transplantation.
We presented KHP 2033 as a future vision for kidney health, with the goal of promoting kidney health for all. Our goals are to prevent the development of ESKD, particularly DKD, and increase the proportion of patients with ESKD receiving home therapy, thereby reducing the socioeconomic burden of kidney disease and improving the quality of patient-centered care.
The missions of KHP 2033 will be realized not only through the efforts of the nephrology society or patients but also through feasible and sustained efforts on the part of healthcare professionals and policymakers.
Notes
Conflicts of interest
All authors have no conflicts of interest to declare.
Data sharing statement
The data presented in this study are available upon reasonable request from the corresponding author.
Authors’ contributions
Conceptualization: CSL, SHP
Data curation, Formal analysis: DHK, YYH
Investigation, Project administration, Supervision: JJC, SL, HKL, JWC, SHK, SYH, CWP, EYL, DRC, SGK, CSL, SHP
Writing–original draft: DHK, YYH, SHP
Writing–review & editing: All authors
All authors read and approved the final manuscript.
Acknowledgements
We would like to thank all the cabinet members in the Korean Society of Nephrology, especially Yong Kyun Kim and Seon Ho Ahn, the directors the KORDS registry, and Hye Eun Yoon, a committee member of the KORDS registry. The authors participated in the Joint Project on Quality Assessment Research, and the Health Insurance Review and Assessment Service collected and provided the claims data and quality assessment data to the authors.