Clinical significance of the living kidney donor profile index for predicting long-term posttransplant outcomes: results from the Korean Organ Transplantation Registry
Article information
Abstract
Background
The usefulness of the living kidney donor profile index (LKDPI) has not been widely demonstrated; therefore, it requires verification before clinical application. We analyzed the LKDPI using data from the Korean Organ Transplantation Registry (KOTRY) to confirm whether the LKDPI can be used to predict the survival of allografts in living donor kidney transplantation (LDKT) patients in Korea.
Methods
The study population was obtained from the KOTRY database. A total of 2,598 kidney recipients registered in the KOTRY database were enrolled between May 2014 and December 2020. Donor and recipient information was observed, and the LKDPI was measured.
Results
Median LKDPI score was 15.5 with a follow-up duration of 33.7 ± 16.1 months. According to LKDPI scores (group 1, <0; group 2, 0–20; group 3, 20–40; and group 4, >40), LKDPI group 4 had significantly higher death-censored graft loss than LKDPI group 1 (hazard ratio [HR], 1.89; 95% confidence interval [CI], 1.06–3.40; p = 0.03). When divided based on the cutoff value (LKDPI, 36.6), the high LKDPI group had higher graft loss than the low LKDPI group (HR, 2.14; 95% CI, 1.37–3.34; p < 0.001). When follow-up was repeated after transplantation, it was confirmed that the higher the LKDPI value was, the lower the average estimated glomerular filtration rate (p < 0.001).
Conclusion
This study confirmed that LKDPI can serve as an independent predictor for assessing the risk of allograft failure and transplant outcomes in Korean LDKT patients.
Introduction
Kidney transplantation is the best renal replacement therapy for patients with end-stage renal disease (ESRD) undergoing dialysis. The number of patients with ESRD is increasing, as is the need for organ donation [1–4]. However, owing to the lack of deceased donor kidneys, the wait time for kidney transplants is also increasing [5–8]. Living donor kidney transplantation (LDKT) is superior to deceased donor kidney transplantation (DDKT) in terms of transplant survival and patient quality of life [9,10]. For this reason, LDKT constitutes a high proportion (40%) of kidney transplants performed worldwide [11].
The prognostic methodology used to predict DDKT outcome according to donor characteristics, such as the kidney donor profile index (KDPI), was established over a long period of time and has facilitated understanding of the risk to transplant recipients, allowing providers to make better clinical decisions [12–18]. A recent study conducted in the United States calculated the living kidney donor profile index (LKDPI) to determine LDKT characteristics and create a graft survival model [19]. LKDPI is calculated by combining certain characteristics of donors and recipients, such as age, weight, body mass index (BMI), estimated glomerular filtration rate (eGFR), and donor/recipient relationship [20–23]. LKDPI allows donors/recipients to receive appropriate kidney transplants in which blood type or cross-matching is appropriate and reduces wait times for transplants through paired kidney donation programs [24,25]. This can be useful for choosing an appropriate donor when there are multiple living donor kidneys.
However, the usefulness of the LKDPI has not been widely demonstrated; it needs to be verified before wider clinical application. As the LKDPI is derived from the United States population alone, whether it can be applied to other populations remains unclear [26]. Whether the LKDPI can be applied in Korea is an open query because there are many differences between the healthcare systems and patient characteristics of the United States and Korea.
In this study, data from the Korean Organ Transplantation Registry (KOTRY) were used to verify the LKDPI through posttransplantation organ results and to derive optimal cutoff values for predicting graft survival.
Methods
Study participants
All data from this study were obtained from an online registry based on the KOTRY electronic health records. KOTRY data are a multicenter, nationwide database established in 2014 to improve the prognosis of organ transplant patients and to help develop national policies through biomarker development among Korean organ transplant patients [27]. Patients undergoing kidney transplantation were registered in the KOTRY database; demographics, laboratory data, dialysis parameters, clinical outcomes, and complications data were collected based on scientific evidence from more than 40 centers. A total of 3,457 patients with LDKT were screened from the KOTRY database between May 2014 and December 2020. Of the 3,457 LDKT patients, 2,598 were included in this study. Three hundred patients whose LKDPI score could not be calculated due to missing variables were excluded and another 559 patients were excluded due to follow-up loss, including withdrawal of consent or transfer to another medical institution (Fig. 1). Written informed consent was achieved from all patients before being enrolled in the study. All study procedures complied with the principles expressed in the Declaration of Helsinki. The study protocol was reviewed and approved by the Institutional Review Board of each center, and the approval number from Kyung Hee University Medical Center is 2020-01-045.
Clinical parameters and outcomes
The primary outcome was death-censored graft loss, defined as the need for dialysis and transplantation, excepting deaths with maintained graft function.
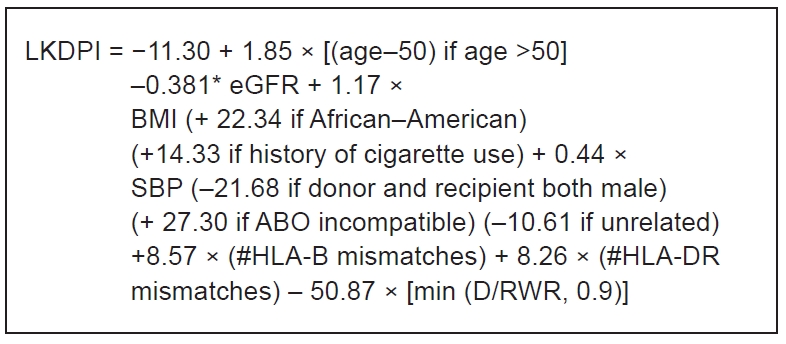
LKDPI scores were calculated as living donor characteristics, and the formula was based on that created by Johns Hopkins Hospital (Fig. 2) (online calculator available at http://www.transplantmodels.com/lkdpi/) [19]. The data were retrospectively analyzed, and the LKDPI score was derived by incorporating the following variables: age, eGFR (as estimated by the Chronic Kidney Disease Epidemiology Collaboration formula), BMI, systolic blood pressure, history of smoking, sex, ethnicity, number of human leukocyte antigen (HLA) mismatches, ABO incompatibility, and donor-recipient weight ratio.
In addition, information such as dialysis before kidney transplantation, average time for renal replacement therapy, previous kidney transplantation history, cold ischemic time, immunosuppressant type, and desensitization history were included in the baseline calculations. We also analyzed eGFR at discharge and 6 months, 1 year, 2 years, 3 years, 4 years, and 5 years after kidney transplantation.
Data analysis
Baseline characteristics and parameters were calculated using mean and standard deviation. Differences between the two groups were identified using Student t test. Categorical variables were compared using the chi-square test or Fisher exact test. The Cox proportional hazard ratio (HR) was used to investigate the relationship between the LKDPI and death-censored graft loss. Cox analysis was performed for each LKDPI score to determine the LKDPI cutoff value. The score with the highest HR among the units was set as the optimal cutoff value. The following factors were selected as confounding variables for multivariable death-censored graft loss analysis: recipient age, diabetes mellitus (DM) status of recipient and donor, use of immunosuppressants after LDKT, induction therapy (antithymocyte globulin) before LDKT, and history of kidney transplantation. Repeated-measures analysis of variance was used to analyze eGFR measured at regular intervals after kidney transplantation. The p-values of <0.05 were considered statistically significant. Statistical analyses were conducted using the R software version 3.6.2 R Foundation for Statistical Computing) and IBM SPSS version 22.0 (IBM Corp.).
Results
Baseline demographic characteristics and laboratory data
The baseline characteristics are shown in Table 1. A total of 2,598 living kidney transplant donors were included in this study.
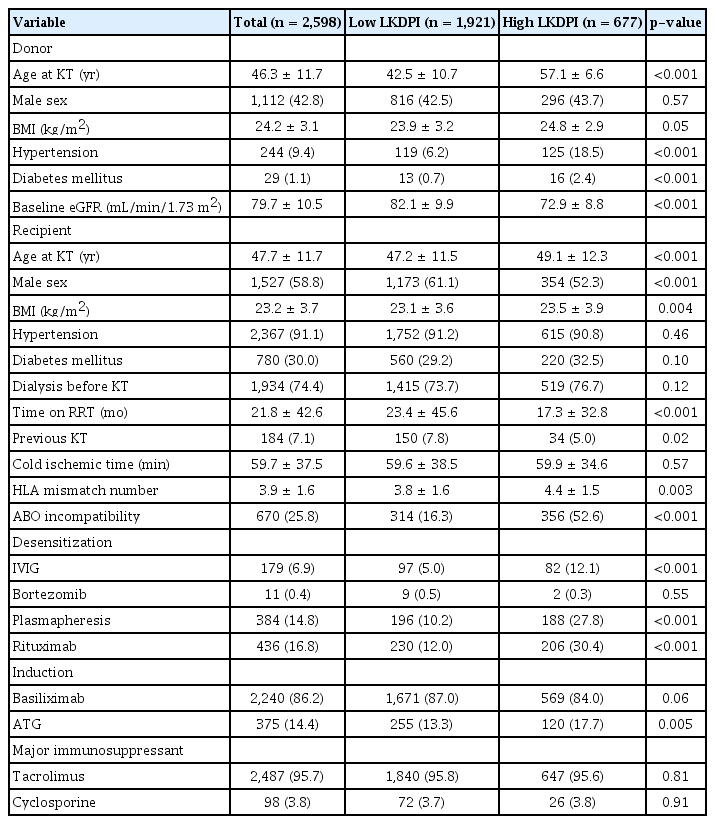
Comparison of clinical and laboratory parameters between high LKDPI donors (or recipients) and low LKDPI donors (or recipients)
Mean donor age was 46.3 ± 11.7 years, and 1,112 patients (42.8%) were male. Mean baseline eGFR was 79.7 ± 10.5 mL/min/1.73 m2, and mean BMI was 24.2 ± 3.1 kg/m2. Of donors, 244 (9.4%) had hypertension and 29 (1.1%) had DM.
Mean recipient age was 47.7 ± 11.7 years, and 1,527 patients (58.8%) were male. The recipients’ mean BMI was 23.2 ± 3.7 kg/m2. Among the recipients, 2,367 (91.1%) had hypertension and 780 (30.0%) had DM. The number of patients who received pretransplantation renal replacement therapy was 1,934 (74.4%), and mean duration was 21.8 ± 42.6 months. In addition, 184 patients (7.1%) underwent preemptive transplants. Mean cold ischemic time was 59.7 ± 37.5 minutes. The HLA mismatch number was 3.9 ± 1.6, and 670 patients (25.8%) had ABO incompatibility. Overall, 14.4% of patients were prescribed a depleting agent for induction treatment (antithymocyte globulin); tacrolimus was the most prescribed calcineurin inhibitor after discharge.
In this study, the cutoff value was obtained by performing Cox analysis for each score to find the best cutoff value for the survival model considering the duration until the event occurred. The optimal cutoff value was 36.6 (HR, 2.23). We divided patients into two groups, low LKDPI (n = 1,921) and high LKDPI (n = 677), based on the cutoff values.
Among the donors, the high LKDPI group (57.1 ± 6.6 years) was significantly older than the low LKDPI group (42.5 ± 10.7 years). There was no significant difference in the sex ratio and mean BMI between the high and low LKDPI groups. The high LKDPI group had a higher proportion of patients with hypertension (18.5% vs. 6.2%) and DM (2.4% vs. 0.7%) than the low LKDPI group. In eGFR, the high LKDPI group was lower than the low LKDPI group (72.9 ± 8.8 mL/min/1.73 m2 vs. 82.1 ± 9.9 mL/min/1.73 m2).
In the recipient group, the high LKDPI group (49.1 ± 12.3 years) was significantly older than the low LKDPI group (47.2 ± 11.5 years). The proportion of males, mean time of renal replacement therapy, and previous kidney transplantation history were significantly lower in the high LKDPI group. In terms of HLA mismatch number, the high LKDPI group was significantly higher than the low LKDPI group (4.4 ± 1.5 vs. 3.8 ± 1.6). ABO incompatibility was also higher in the high LKDPI group than in the low LKDPI group (52.6% vs. 16.3%).
Graft survival according to living kidney donor profile index
The distribution of the LKDPI scores is presented in Fig. 3. The median LKDPI was 15.5, with LKDPI values ranging from –80.7 to 118.6.
A total of 82 cases of death-censored graft loss were noted during the follow-up period. Median follow-up duration was 33.7 ± 16.1 months. When LDKT patients were divided into four groups according to LKDPI scores (group 1, <0; group 2, 0–20; group 3, 20–40; and group 4, >40), group 4 had more significant graft loss in univariate (HR, 2.06; 95% confidence interval [CI], 1.16–3.68; p = 0.01) and multivariate (HR, 1.89; 95% CI, 1.06–3.40; p = 0.03) analyses than group 1, as shown in Table 2 and Fig. 4. With each unit increase in LKDPI, death-censored graft loss also increased in the univariate (HR, 1.01; 95% CI, 1.00–1.02; p = 0.02) and multivariate studies (HR, 1.01; 95% CI, 1.00–1.02; p = 0.045). When drawing a cubic spline curve based on this, LKDPI and graft loss were closely related (Fig. 5).
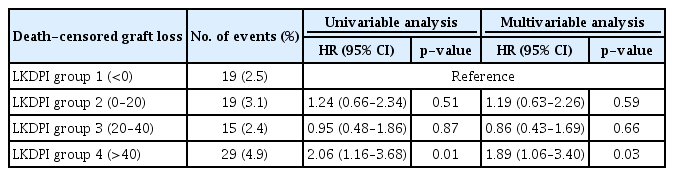
Univariate and multivariate Cox regression analysis for LKDPI quartile groups with an elevated risk of death-censored graft loss
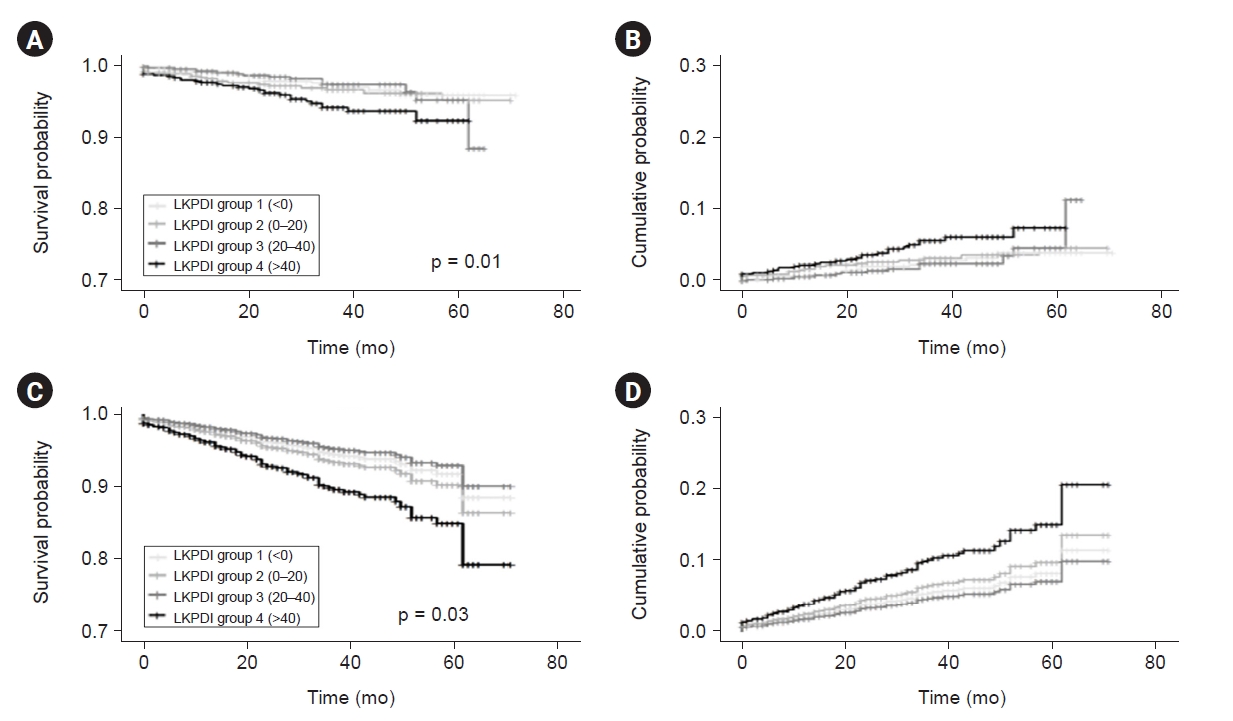
Recipient survival probability and cumulative probability of death-censored graft loss after living donor kidney transplantation by LKDPI quartile group.
(A, B) Univariate analysis. (C, D) Multivariate analysis. LKDPI, living kidney donor profile index.

Cubic spline curve between LKDPI and hazard ratio.
(A) Univariable analysis. (B) Multivariable analysis. LKDPI, living kidney donor profile index.
The cutoff value of LKDPI calculated using Cox analysis was 36.6. Based on the cutoff value, inclusion in the high LKDPI group was a significant risk factor for graft failure in the univariate model (HR, 2.23; 95% CI, 1.44–3.46; < 0.001) as well as in the multivariate model (HR, 2.14; 95% CI, 1.37–3.34; < 0.001) (Table 3, Fig. 6).

Univariate and multivariate Cox regression analysis between low LKDPI and high LKDPI groups divided by cutoff value with an elevated risk of death-censored graft loss

Recipient survival probability of death-censored graft loss after living donor kidney transplantation between the high and low LKDPI groups.
(A) Univariable analysis. (B) Multivariable analysis. CI, confidence interval; HR, hazard ratio; LKDPI, living kidney donor profile index.
As a result of the receiver operating characteristic analysis, the area under the curve was 0.57 (95% CI, 0.50–0.63; p = 0.03), and the resulting cutoff value was 33.2. Even when analyzed based on this cutoff value, the high LKDPI group showed significantly higher death-censored graft loss than the low LKDPI group (HR, 1.86; 95% CI, 1.20–2.89; p = 0.01).
Long-term graft function according to living kidney donor profile index
The eGFR was measured at discharge and at 6 months, 1 year, 2 years, 3 years, 4 years, and 5 years in the low and high LKDPI groups. The high LKDPI group maintained a lower average eGFR after kidney transplantation than the low LKDPI group (Fig. 7). Considering the interaction between time and LKDPI, the high LKDPI group showed a pattern in which eGFR value decreased rapidly compared with the low LKDPI group in univariate and multivariate analyses (p < 0.001) (Table 4).

Average eGFR in the high and low LKDPI groups after living donor kidney transplantation.
eGFR, estimated glomerular filtration rate; LKDPI, living kidney donor profile index.
Discussion
Since organs for kidney transplantation are always in short supply, a tool that could compare the quality of living donor kidneys would facilitate efficient use. Because there is a wide disparity of quality among donor kidneys, predicting the outcome after kidney transplantation with consideration for the initial donor condition is a crucial issue for LDKT. Therefore, Massie et al. [19] developed the LKDPI, which was designed to anticipate the possibility of graft loss using the characteristics of living donors and recipients.
In Korea, research has been conducted to determine whether the KDPI can be used to predict clinical outcomes after transplantation in patients with DDKT. The study confirmed that KDPI can be a useful indicator for predicting the outcomes of patients with DDKT [28]. However, the LKDPI is a relatively recent tool in clinical decision-making, and it is important to ensure that this index be evaluated for effectiveness in varied cohorts before implementing it to clinical use [29]. Therefore, we conducted external verification of the LKDPI in a Korean cohort. As few studies on LKDPI have been conducted in Asia, especially in Korea, this study is meaningful considering the usefulness of LKDPI over a long time based on a large cohort.
In this study, we evaluated whether a high LKDPI score is associated with an increased risk of death-censored graft loss in Korea, similar to a large United States cohort study. According to a previous study based on a European cohort published in 2019, a quartile analysis of LDKT patients showed that graft loss significantly increased in the highest LKDPI group, with an LKDPI score of ≥33 [30]. It is still controversial whether the same score of 33 can be applied to Korea, but the optimal cutoff value (36.6) was similar to that of Germany through Cox analysis conducted based on KOTRY data [30].
The LKDPI seems to be a powerful tool for predicting graft failure based on the Korean database; these results were based on dichotomies based on cutoff values and LKDPI scores. LKDPI is beneficial because recipients are given the option to choose when they have multiple transplant donor candidates. In this respect, LKDPI enables patients who receive transplants to recognize the risks associated with living donors.
Although this study is based on a large, long-term cohort, the number of events in death-censored graft loss was small. Another method to compensate for this small number of events is needed. Therefore, we continued to track the eGFR of patients who underwent LDKT through blood tests in the outpatient clinic after discharge, and the results were analyzed through repeated measurements. When eGFR was reexamined 6 months, 1 year, 2 years, 3 years, 4 years, and 5 years after hospital discharge, the group with a higher LKDPI had a lower eGFR than the group with a lower LKDPI, and it decreased faster over time.
Furthermore, since the LKDPI showed some predictability across cohorts, we expect to further improve the generalization of the model by including potentially important new predictors or by using updated cohorts. Several studies have shown that donor age in LDKT is a predictor of graft survival after transplantation [21,31]. Among them, Massie et al. [19] showed that all causes of graft loss significantly increase in LDKT if the donor age is over 50 years. In our cohort, there were no clinically significant results when patients were divided into subgroups based on age of ≥50 years, and death-censored graft loss was analyzed (HR, 1.351; 95% CI, 0.865–2.110; p = 0.19). However, since the proportion of people aged ≥50 years is high (58%) in KOTRY’s living donation cohort, it is also important to check the relationship between graft survival and age when data are accumulated through long-term follow-up. Considering the results of previous studies, some factors are not included in the LKDPI formula but can affect LDKT outcomes. Comorbid diseases, such as cardiovascular disease, DM, and time on dialysis have significant impacts on the survival rate of grafts [32–34]. If LKDPI can be supplemented to incorporate these comorbidities, the prognosis of patients after LDKT can be more accurately predicted.
This study has some limitations. First, the formula used to calculate the LKDPI in this study was constructed at Johns Hopkins University of the United States [19] and includes a variable that can be applied to African Americans, but it is unknown whether the formula applies well to Asians, and especially to Koreans. Second, this study predicted prognosis using the retrograded LKDPI in patients who received transplants. Since the LKDPI was originally a prospective predictor, retrospective studies may experience distortion of the results due to bias. In addition to the quality of the donor identified by the LKDPI, the prognosis may vary due to the clinical state of the recipient and the determinations of clinicians; therefore, it is necessary to verify the predictive power of the LKDPI through prospective research. Third, it is possible that our study was affected by the missing data.
In conclusion, LKDPI was found to be useful in evaluating prognosis after kidney transplantation in the LDKT cohort in Korea. Although the LKDPI was created and evaluated based on the United States data, it can be an effective tool for evaluating donor kidneys in other countries and other medical environments. Based on long-term, large population cohort data, impressive results can be obtained using LKDPI to predict prognosis after LDKT.
Notes
Conflicts of interest
All authors have no conflicts of interest to declare.
Funding
KOTRY cohort was funded by the Research of Korea Centers for Disease Control and Prevention Agency (2014-ER6301-00, 2014-ER6301-01, 2014-ER6301-02, 2017-ER6301-00, 2017-ER6301-01, 2017-ER6301-02, 2020-ER7201-00). This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (NRF-2021R1A2C1012120).
Data sharing statement
The data presented in this study are available on request from the corresponding author.
Authors’ contributions
Conceptualization: KHJ
Data curation, Investigation: CWJ, DGK, YHK, JY, CA; the Korean Organ Transplantation Registry Study Group
Formal analysis: JHK, KHJ
Funding acquisition: KHJ
Methodology, Validation: SHL, JSK, HSH, HK
Writing–original draft: KHJ, JHK
Writing–review & editing: All authors
All authors read and approved the final manuscript.
Acknowledgements
KOTRY was established in 2014 and has managed nationwide cohorts of kidney, liver, pancreas, heart, and lung transplants. The kidney subcommittee consisted of 41 researchers from 39 transplant centers. The names of the KOTRY participating hospitals and principal investigators of the kidney subcommittee are as follows: BHS Hanseo Hospital (Jin Min Kong), Han Yang University Hospital (Oh Jung Kwon), Korea University Anam Hospital (Myung-Gyu Kim, Cheol-Woong Jung), Wonju Severance Christian Hospital (Sung Hoon Kim), Inje University Busan Paik Hospital (Yeong Hoon Kim), Bongseng Memorial Hospital (Joong Kyung Kim), Kyungpook National University Hospital (Chan-Duck’Kim), Bucheon St. Mary’s Hospital (Ji Won Min), Chonbuk National University Hospital (Sung Kwang Park), Gil Medical Center (Yeon Ho Park), Ajou University Hospital (Inwhee Park), Samsung Medical Center (Park Jae Berm), Konkuk University Hospital (Jung Hwan Park), Yeungnam University Hospital (Jong-Won Pa’k), Eunpyeong St. Mary’s Hospital (Tae Hyun Ban), Pusan National University Hospital (Sang Heon Song), Ewha Womans University Medical Center (Seung Hwan Song), Kosin University Gaspel Hospital (Ho Si’ Shin), Seoul St. Mary’s Hospital (Chul Woo Yang), Incheon St. Mary’s Hospital (Hye Eun Yoon), Chungnam National University Hospital (Kang Wook Lee), Maryknoll Medical Center (Dong Ryeol Lee), Pusan National University Yangsan Hospital (Dong Won Lee), Kangdong Sacred Heart Hospital (Samuel Lee), Kyung Hee University Hospital at Gangdong (Sang Ho Lee), CHA Bundang Medical Center (Yu Ho Lee), SNU Boramae Medical Center (Jung Pyo Lee), Myongji Hospital (Jeong-Hoon Lee), Soonchunhyang University Seoul Hospital (Jin Seok Jeon), Inje University Ilsan Paik Hospital (Heungman Jun), Kyung Hee University Hospital (Kyung Hwan Jeong), Ewha Womans University Mokdong Hospital (Ku Yong Chung), Ulsan University Hospital (Hong Rae Cho), Gangnam Severance Hospital (Man Ki Ju), Seoul National University Bundang Hospital (Dong-Wan Chae), Chonnam National University Hospital (Soo Jin Na Choi), Asan Medical Center (Duck Jong Han), Keimyung University School of Medicine (Seungyeup Han), Severance Hospital (Jaeseok Yang, Kyu Ha Huh), and Seoul National University Hospital (Curie Ahn).