Dialysis modality-related disparities in sudden cardiac death: hemodialysis versus peritoneal dialysis
Article information
Abstract
Background
Patients require risk stratification and preventive strategies for sudden cardiac death (SCD) based on the dialysis modality because the process of dialysis is a risk factor for SCD. This study aimed to compare the risk of SCD in patients undergoing hemodialysis (HD) versus peritoneal dialysis (PD).
Methods
Patients on HD and PD were included in the end-stage renal disease registry of the Korean Society of Nephrology between 1985 and 2017. The incidence and associated factors of SCD were analyzed based on the dialysis modality.
Results
Of 132,083 patients, 34,632 (26.2%) died during 94.8 ± 73.6 months of follow-up. In patients on HD and PD, 22.2% and 19.6% of total deaths were SCDs. In the propensity score-matched population, SCD accounted for 21.7% and 19.6% of total deaths in patients on HD and PD, respectively. HD was independently associated with SCD even after adjusting for age and significant comorbidities. Hypertension, coronary artery disease, and congestive heart failure, and age at the time of death < 65 years were independent risk factors for SCD in patients on HD but not in those on PD. Diabetes was significantly associated with SCD regardless of the dialysis modality.
Conclusion
Compared with patients on PD, Korean patients on HD have a higher risk of SCD, which is attributable to cardiac comorbidities.
Introduction
Sudden cardiac death (SCD) accounted for 25% of the total mortality of dialysis patients in previous large-scale prospective studies [1,2]. Because SCD constitutes a considerable proportion for all causes of death in patients with end-stage renal disease (ESRD) [3,4], SCD should receive more attention to clarify risk factors. Furthermore, more preventive interventions for SCD are required to improve patient survival.
The pathophysiology of SCD in patients undergoing dialysis has been known to be different from that in the general population. A previous study has shown that left ventricular hypertrophy plays a major role in the occurrence of SCD rather than traditional cardiovascular risk factors [5]. In patients undergoing hemodialysis (HD), large electrolyte [6–9] and fluid shifts [10,11] and non-ventricular arrhythmias [8,12,13] during dialysis have been known to be contributors to SCD. Considering that the process of dialysis is one of the risk factors of SCD in dialysis patients, and both HD and peritoneal dialysis (PD) are fundamentally different in terms of continuity and rapidity, risk stratification and preventive strategies for SCD based on the dialysis modality are required. Data regarding the result of SCD comparing HD and PD are limited [4].
The present study aimed to investigate the incidence of SCD and associated risk factors for SCD based on the dialysis modality (HD versus PD) from the Korean Society of Nephrology (KSN) ESRD registry.
Methods
Study design and participants
The KSN ESRD Registry Committee has registered Korean patients on dialysis and collected dialysis data since 1985. The mean response rate of the KSN ESRD registry has reached approximately 70% [14]. This retrospective study was conducted using data on patients on HD and PD registered in the KSN ESRD registry between 1985 and 2017. After patients with insufficient data were excluded, 34,632 of 132,083 enrolled patients were died during the follow-up period (27,158 of HD and 7,474 of PD). The initial dialysis modality was used to analyze, and subsequent switching of dialysis modality was not considered.
Definition of SCD and associated factors with SCD
Death causes were derived from the KSN ESRD registry report. SCD was defined as deaths coded as “cardiac arrest-related uremia” or “cardiac arrest-unrelated uremia.” Cardiac arrest due to coronary artery disease was excluded from SCD. Other causes of death include cardiac death due to coronary artery disease, vascular death (including cerebrovascular disease, pulmonary embolism, gastrointestinal bleeding, gastrointestinal embolism, etc.), infection-related death (including pneumonia, sepsis, tuberculosis, peritonitis, etc.), hepatic failure, social causes (including denial of treatment due to economic causes, denial of treatment other than economic causes, and suicide), and others (including malnutrition, malignant tumors, accidental accidents, etc.).
The dialysis modality, age at the time of dialysis initiation and death, sex, duration of dialysis, and presence of comorbidities, including diabetes mellitus, hypertension, coronary artery disease, congestive heart failure, and arrhythmia were obtained as factors possibly associated with SCD. The most recent information regarding the comorbidities was obtained. The causes of death and co-morbidities were determined by the physicians’ clinical judgment.
Statistical analysis
Demographic and clinical data were compared using Pearson’s chi-squared test or Fisher’s exact test for categorical variables and Student’s t test for continuous variables between HD and PD population. Continuous variables were expressed as mean ± standard deviation. Chi-squared test was used to analyze the percentage of SCD from the total deaths based on the dialysis modality. Multivariate logistic regression analysis was used to investigate the association between dialysis modality and background variables and SCD. A propensity score-matched analysis was performed, wherein the model was reconstructed using age, sex, duration of dialysis, presence of diabetes, hypertension, coronary artery disease, congestive heart failure, pericardial effusion, arrhythmia, and cerebrovascular accident. The percentage of missing data on the duration of dialysis was 0.7%, which was excluded from the analysis. No information was missing on age, sex, and comorbidities. Statistical analysis was performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA). Statistical significance was determined by P < 0.05.
Results
Characteristics of non-survivors based on the dialysis modality
Table 1 demonstrates the baseline characteristics of the entire patient population and propensity score-matched patients based on the dialysis modality. In the entire non-survivors, patients on HD were older at the time of death, had a longer duration of dialysis, and had a higher proportion of males, hypertension, coronary artery disease, congestive heart failure, pericardial effusion, arrhythmia, and cerebrovascular disease than patients on PD. No differences in baseline characteristics were observed in the matched population.
Causes of death
Table 2 shows the causes of death in the entire patient population and propensity score-matched patients based on the dialysis modality. SCD accounted for 22.2% and 19.6% of overall HD and PD deaths, respectively. In the propensity score-matched population, SCD accounted for 21.7% and 19.6% of HD and PD deaths, respectively.
Characteristics of patients based on the cause of death
Of 132,083 patients, 34,632 (26.2%) patients died during the 94.8 ± 73.6 months of follow-up. This included 7,493 (21.6%) and 27,139 (78.4%) patients who had SCD and non-SCD, respectively. In the matched population, 3,076 (20.6%) and 11,828 (79.4%) patients died because of SCD and non-SCD, respectively.
Table 3 shows the demographic and clinical characteristics of patients based on the cause of death. The mean age of the SCD group was 60.4 years, and 58.2% were male. This included 80.5% and 57.9% of the SCD group who underwent HD and had diabetes as a cause of ESRD. The SCD group was significantly younger (P = 0.002) and had a higher proportion of HD (P < 0.001), diabetes (P < 0.001), hypertension (P < 0.001), coronary artery disease (P < 0.001), congestive heart failure (P < 0.001), and arrhythmia (P < 0.001) compared with the non-SCD group. No differences were observed in pericardial effusions and cerebrovascular accidents between the two groups. In the propensity score-matched patients, the SCD group had a higher proportion of HD (P = 0.001), diabetes (P = 0.002), hypertension (P = 0.016), coronary artery disease (P = 0.032), and congestive heart failure (P = 0.004) compared with the non-SCD group.
Comparison of the proportion of SCD between dialysis modality
Fig. 1 shows the percentage of SCD among the total deaths based on the dialysis modality of the entire population, matched population, and subgroups. In the entire population, the proportion of SCD in patients on HD was significantly higher than that in patients on PD (HD vs. PD: 22.2 vs. 19.6%, P < 0.001). In the matched population, the proportion of SCD in patients on HD was significantly higher than that in patients on PD (HD vs. PD: 21.7 vs. 19.6%, P = 0.001). In subgroups, the percentage of SCD in patients on HD was also higher than that in those on PD who were ≥ 65 years (HD vs. PD: 21.4 vs. 18.7%, P = 0.002), < 65 years (HD vs. PD: 22.8 vs. 20.0%, P < 0.001), male (HD vs. PD: 21.9 vs. 19.2%, P < 0.001), female (HD vs. PD: 22.7 vs. 20.1%, P = 0.002), had diabetes (HD vs. PD: 23.6 vs. 20.5%, P < 0.001), and hypertension (HD vs. PD: 24.2 vs. 19.8%, P < 0.001).
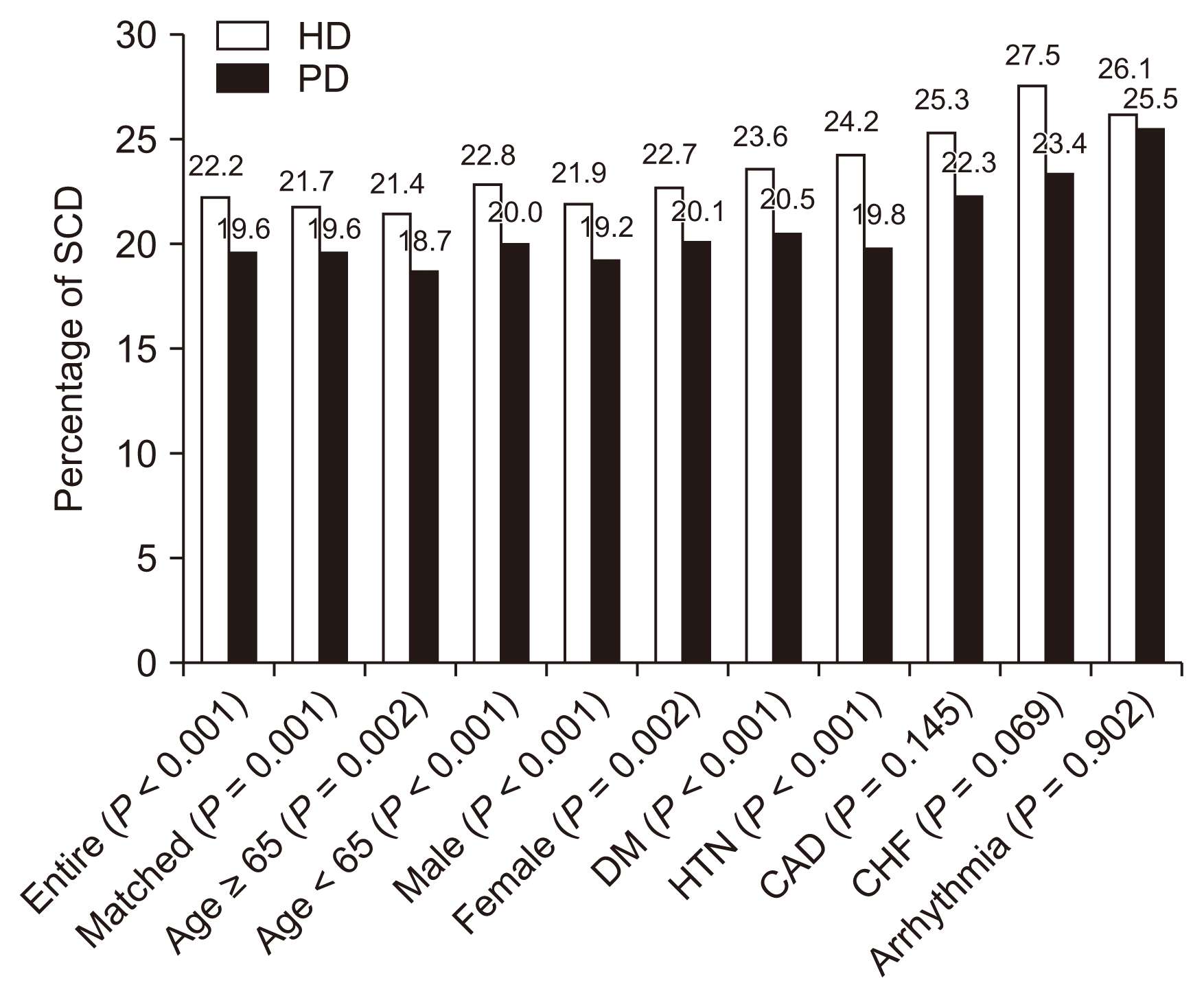
Percentage of sudden death in different subgroups: hemodialysis (HD) versus peritoneal dialysis (PD).
In the entire population, the proportion of sudden In subgroups, the percentage of sudden cardiac death (SCD) in patients on HD was still higher than that in patients on PD who were ≥65 years, < 65 years, male, female, had diabetes, and hypertension.
CAD, coronary artery disease; CHF, congestive heart failure; DM, diabetes mellitus; HTN, hypertension.
Analysis of factors associated with SCD
Table 4 shows the univariate and multivariate analysis results for SCD. Univariate analysis showed that HD (odds ratio [OR], 1.17; 95% confidence interval [CI], 1.10–1.25; P < 0.001), age at the time of death < 65 years (OR, 1.09; 95% CI, 1.03–1.14; P = 0.002), female (OR, 1.10; 95% CI, 1.00–1.11; P = 0.065), diabetes (OR, 1.18; 95% CI, 1.12–1.25, P < 0.001), hypertension (OR, 1.20; 95% CI, 1.14– 1.27, P < 0.001), coronary artery disease (OR, 1.22; 95% CI: 1.13–1.33, P < 0.001), congestive heart failure (OR, 1.39; 95% CI, 1.28–1.50, P < 0.001), and arrhythmia (OR, 1.29; 95% CI, 1.15–1.45, P < 0.001) were significantly associated with SD.
Multivariate analysis showed that HD (OR, 1.15; 95% CI, 1.08–1.23, P < 0.001), age at the time of death < 65 years (OR, 1.09; 95% CI: 1.01–1.18; P = 0.028), diabetes (OR, 1.17; 95% CI, 1.11–1.24; P < 0.001), hypertension (OR, 1.12; 95% CI. 1.06–1.19; P < 0.001), coronary artery disease (OR, 1.10; 95% CI, 1.01–1.20; P = 0.025), congestive heart failure (OR, 1.27; 95% CI, 1.16–1.38; P < 0.001), and arrhythmia (OR, 1.14; 95% CI, 1.01–1.29; P = 0.029) were independent risk factors for SCD.
Analysis of factors associated with SCD based on the dialysis modality
Table 5 shows the univariate and multivariate analysis results for SCD in patients on HD and PD. Univariate analysis showed that age at the time of death < 65 years (OR, 1.11; 95% CI, 1.05–1.18, P < 0.001), diabetes (OR, 1.20; 95% CI, 1.13–1.27; P < 0.001), hypertension (OR, 1.22; 95% CI, 1.15–1.29; P < 0.001), coronary artery disease (OR, 1.21; 95% CI, 1.11–1.32; P < 0.001), congestive heart failure (OR, 1.38; 95% CI, 1.27–1.51; P < 0.001), and arrhythmia (OR, 1.25; 95% CI, 1.11–1.41, P < 0.001) were significantly associated with SCD in patients on HD. Diabetes (OR, 1.14, 95% CI, 1.01–1.28; P = 0.028) and congestive heart failure (OR, 1.28; 95% CI, 1.02–1.60; P = 0.034) were significantly associated with SCD in patients on PD. Multivariate analysis showed that age at the time of death < 65 years (OR, 1.12; 95% CI, 1.03–1.22; P = 0.011), diabetes (OR, 1.18; 95% CI, 1.11–1.25; P < 0.001), hypertension (OR, 1.16; 95% CI, 1.09–1.24; P < 0.001), coronary artery disease (OR, 1.10; 95% CI, 1.00–1.21; P = 0.048), and congestive heart failure (OR, 1.27; 95% CI, 1.16–1.40; P < 0.001) were independent risk factors for SCD in patients on HD. Diabetes was independently associated with SCD in patients on PD (OR, 1.16; 95% CI, 1.03–1.30; P = 0.016).
Comparison of the proportion of SCD based on the years
Fig. 2 shows the percentage of SCD among the total deaths based on the years. In patients on HD, the proportion of SCD between 2001 and 2017 was significantly higher than that between 1985 and 2000 (2001–2017 vs. 1985–2000: 22.6 vs. 17.9%, P = 0.008). The proportion of SCD based on the years was not significantly different in patients on PD.

Different percentages of sudden cardiac death according to the years.
In patients on hemodialysis (HD), the proportion of sudden cardiac death (SCD) between 2001 and 2017 was significantly higher than that between 1985 and 2000 (2001–2017 vs. 1985–2000: 22.6 vs. 17.9%, P = 0.008). The proportion of SCD based on the years was not significantly different in patients on peritoneal dialysis (PD).
Discussion
The present study using data from the nationwide KSN ESRD registry showed that SCD was more common in Korean patients on HD compared with those on PD, accounting for 22.2% and 19.6% of all deaths, respectively, which was consistent with the propensity score-matched population. We further showed that age < 65 years and cardiac comorbidities (including hypertension, coronary artery disease, and congestive heart failure) had a negative impact on SCD only in patients on HD, but not in those on PD. Patients with diabetes were vulnerable to SCD regardless of the dialysis modality.
To date, no universally accepted definition of SCD has existed. SCD has been defined as a natural, rapid, and unexpected cardiac death within an hour of symptom onset [3]. However, determining the information on the clinical circumstances surrounding death and timing of death from symptom onset of dialysis patients is difficult in real clinic practice. Furthermore, the results of the autopsy series of 93 patients on dialysis clinically classified as having SCD showed that the most common cause was stroke [15]. Therefore, we admitted not being completely free from the potential for misclassification of SCD and defined SCD as either cardiac arrest-related or unrelated uremia. The incidence of SCD in patients with ESRD is approximately 100 times higher than that in the general population at approximately 0.41 per 1,000 and 0.27 per 1,000 patient years in males and females, respectively [16]. Contrary to our study results, a previous on SCD comparing HD and PD showed that SCD accounted for 12.1% and 22.8% of all causes of death in patients on HD and PD, respectively, and the incidence of SCD was independent of the dialysis modality [4]. This might be explained by the difference in the study population and the definitions of SCD.
In our study, diabetes was significantly associated with SCD regardless of the dialysis modality. Diabetes has been well-recognized to be associated with SCD [17]. Our findings are consistent with those of another study that showed that long (2-day) interdialytic interval led to a higher mortality rate, and this phenomenon had been further maximized in cases of diabetes [18]. Furthermore, diabetes is frequently related to cardiac disease, and this comorbidity has been presumed to increase the risk for SCD.
The notable finding of this study was that hypertension, coronary artery disease, and congestive heart failure were significantly associated with SCD in patients on HD, but not in those on PD. Contrary to patients on PD who maintained a relatively stable volume and electrolyte status owing to the continuous nature of PD, patients on HD experience rapid fluctuations in volume and electrolyte status because of the intermittent properties of HD. Furthermore, the procedure of HD can lead to subclinical myocardial ischemia, which may trigger arrhythmias and cardiac failure [19–21]. In concordance with this clinical evidence, a previous study has reported that patients on PD had less variability in the pattern of cardiac death compared with patients on HD [22]. In addition to the hemodynamic instability of the HD procedure, individual medical conditions, including hypertension and congestive heart failure, might put acute stress on the cardiovascular system in patients on HD and greater risk for SCD than those on PD. However, we cannot completely exclude the possibility that the discrepant impact of cardiac comorbidities and age on SCD based on the dialysis modality might be due to the less occurrence of SCD in patients on PD, which led to statistical insignificance. Contrary to the previous study [8], our study showed that age < 65 years was significantly associated with SCD in patients on HD. Although the exact mechanism behind the association between younger age and SCD has not been clarified, younger patients may tend to have better nutritional status, possibly resulting in increased interdialytic weight gain, volume overload, elevated blood pressure, and electrolyte disturbance, which could play a role in the development of SCD. To clarify this point, further study is needed to determine the association among age, volume status, electrolyte imbalance, and SCD.
The present study has limitations worth mentioning. First, misclassification of the cause of death and unreported comorbidities cannot be completely excluded because the cause of death and comorbidity coding did not undergo external audit. Second, although we tried to adjust significant confounding factors for SCD, unadjusted variables may have persisted. Third, results have been affected by selection bias cannot be excluded because the choice of dialysis modality has not been randomized. Despite these limitations, our data showed that SCD accounts for a considerable proportion of total deaths in dialysis patients and suggests the differential role of cardiac comorbidities on SCD based on the dialysis modality.
In conclusion, Korean patients on HD compared with those on PD had a higher risk for SCD. More attention to managing cardiac comorbidities, including hypertension, coronary artery disease, and congestive heart failure in younger patients on HD, should be required to reduce the risk of SCD and ultimately improve long-term patient survival in dialysis patients.
Acknowledgments
This research was supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute, which is funded by the Ministry of Health and Welfare, Republic of Korea (HC15C1129).
We would like to express our gratitude to the KSN ESRD Registry Committee for providing the registry data for this research.
Notes
Conflicts of interest
All authors declare no competing interests.
Authors’ contributions
Hee-Yeon Jung, Dong-Ryeol Ryu, and Yong-Lim Kim participated in the study design. Hee-Yeon Jung, Ji-Young Choi, Jang-Hee Cho, Sun-Hee Park, Chan-Duck Kim, Dong-Ryeol Ryu, and Yong-Lim Kim participated in the data collection. Hee-Yeon Jung, Hyungyun Choi, Dong-Ryeol Ryu, and Yong-Lim Kim performed the statistical analysis and interpretation of data. Hee-Yeon Jung and Yong-Lim Kim wrote the manuscript. All authors read and approved the final manuscript.




