1. Kovesdy CP. Epidemiology of chronic kidney disease: an update 2022.
Kidney Int Suppl (2011) 2022;12:7ŌĆō11.



2. Tummalapalli SL, Anderson GF. Comparative health care spending for dialysis: an example of public cost containment?
J Am Soc Nephrol 2021;32:2103ŌĆō2104.



4. Ulasi II, Awobusuyi O, Nayak S, et al. Chronic kidney disease burden in low-resource settings: regional perspectives.
Semin Nephrol 2022;42:151336.


5. Sundstr├Čm J, Bodegard J, Bollmann A, et al. Prevalence, outcomes, and cost of chronic kidney disease in a contemporary population of 2ŌĆó4 million patients from 11 countries: the CaReMe CKD study.
Lancet Reg Health Eur 2022;20:100438.



6. Denic A, Rule AD, Glassock RJ. Healthy and unhealthy aging on kidney structure and function: human studies.
Curr Opin Nephrol Hypertens 2022;31:228ŌĆō234.



7. Jiang A, Song A, Zhang C. Modes of podocyte death in diabetic kidney disease: an update.
J Nephrol 2022;35:1571ŌĆō1584.



9. Schell C, Huber TB. The evolving complexity of the podocyte cytoskeleton.
J Am Soc Nephrol 2017;28:3166ŌĆō3174.



10. Reynolds PA. The mechanobiology of kidney podocytes in health and disease.
Clin Sci (Lond) 2020;134:1245ŌĆō1253.



12. Nisoli E, Falcone S, Tonello C, et al. Mitochondrial biogenesis by NO yields functionally active mitochondria in mammals.
Proc Natl Acad Sci U S A 2004;101:16507ŌĆō16512.



13. Qin X, Zhao Y, Gong J, et al. Berberine protects glomerular podocytes via inhibiting Drp1-mediated mitochondrial fission and dysfunction.
Theranostics 2019;9:1698ŌĆō1713.



14. Li W, Du M, Wang Q, et al. FoxO1 promotes mitophagy in the podocytes of diabetic male mice via the PINK1/Parkin pathway.
Endocrinology 2017;158:2155ŌĆō2167.


15. Li SY, Susztak K. The role of peroxisome proliferator-activated receptor ╬│ coactivator 1╬▒ (PGC-1╬▒) in kidney disease.
Semin Nephrol 2018;38:121ŌĆō126.



16. Coughlan MT, Higgins GC, Nguyen TV, et al. Deficiency in apoptosis-inducing factor recapitulates chronic kidney disease via aberrant mitochondrial homeostasis.
Diabetes 2016;65:1085ŌĆō1098.



17. Inoue T, Maekawa H, Inagi R. Organelle crosstalk in the kidney.
Kidney Int 2019;95:1318ŌĆō1325.


18. Brinkkoetter PT, Bork T, Salou S, et al. Anaerobic glycolysis maintains the glomerular filtration barrier independent of mitochondrial metabolism and dynamics.
Cell Rep 2019;27:1551ŌĆō1566.



19. Luo Q, Liang W, Zhang Z, et al. Compromised glycolysis contributes to foot process fusion of podocytes in diabetic kidney disease: role of ornithine catabolism.
Metabolism 2022;134:155245.


21. Qi W, Keenan HA, Li Q, et al. Pyruvate kinase M2 activation may protect against the progression of diabetic glomerular pathology and mitochondrial dysfunction.
Nat Med 2017;23:753ŌĆō762.


22. Chen Z, Zhu Z, Liang W, et al. Reduction of anaerobic glycolysis contributes to angiotensin II-induced podocyte injury with foot process effacement.
Kidney Int 2023;103:735ŌĆō748.


23. Liu C, Wu J, Zhu J, et al. Lactate inhibits lipolysis in fat cells through activation of an orphan G-protein-coupled receptor, GPR81.
J Biol Chem 2009;284:2811ŌĆō2822.


25. Shen J, Wang R, He Z, et al. NMDA receptors participate in the progression of diabetic kidney disease by decreasing Cdc42-GTP activation in podocytes.
J Pathol 2016;240:149ŌĆō160.



26. Thangaraju M, Ananth S, Martin PM, et al. c/ebpdelta Null mouse as a model for the double knock-out of slc5a8 and slc5a12 in kidney.
J Biol Chem 2006;281:26769ŌĆō26773.

27. Nagasawa K, Nagai K, Sumitani Y, et al. Monocarboxylate transporter mediates uptake of lovastatin acid in rat cultured mesangial cells.
J Pharm Sci 2002;91:2605ŌĆō2613.


28. Yang Q, Hu J, Yang Y, et al. Sirt6 deficiency aggravates angiotensin II-induced cholesterol accumulation and injury in podocytes.
Theranostics 2020;10:7465ŌĆō7479.



29. Ahmed K, Tunaru S, Tang C, et al. An autocrine lactate loop mediates insulin-dependent inhibition of lipolysis through GPR81.
Cell Metab 2010;11:311ŌĆō319.


30. Lubojemska A, Stefana MI, Sorge S, et al. Adipose triglyceride lipase protects renal cell endocytosis in a Drosophila dietary model of chronic kidney disease.
PLoS Biol 2021;19:e3001230.



31. Chen W, Jiang Y, Han J, et al. Atgl deficiency induces podocyte apoptosis and leads to glomerular filtration barrier damage.
FEBS J 2017;284:1070ŌĆō1081.



32. Wang Q, Zhao B, Zhang J, et al. Faster lipid ╬▓-oxidation rate by acetyl-CoA carboxylase 2 inhibition alleviates high-glucose-induced insulin resistance via SIRT1/PGC-1╬▒ in human podocytes.
J Biochem Mol Toxicol 2021;35:e22797.



34. Vogtl├żnder NP, Dijkman H, Bakker MA, Campbell KP, van der Vlag J, Berden JH. Localization of alpha-dystroglycan on the podocyte: from top to toe.
J Histochem Cytochem 2005;53:1345ŌĆō1353.



35. Verma R, Venkatareddy M, Kalinowski A, et al. Nephrin is necessary for podocyte recovery following injury in an adult mature glomerulus.
PLoS One 2018;13:e0198013.



36. Sever S, Reiser J. CD2AP, dendrin, and cathepsin L in the kidney.
Am J Pathol 2015;185:3129ŌĆō3130.



37. Koop K, Eikmans M, Wehland M, et al. Selective loss of podoplanin protein expression accompanies proteinuria and precedes alterations in podocyte morphology in a spontaneous proteinuric rat model.
Am J Pathol 2008;173:315ŌĆō326.



38. Torban E, Braun F, Wanner N, et al. From podocyte biology to novel cures for glomerular disease.
Kidney Int 2019;96:850ŌĆō861.


39. Nielsen JS, McNagny KM. The role of podocalyxin in health and disease.
J Am Soc Nephrol 2009;20:1669ŌĆō1676.


41. Ning L, Suleiman HY, Miner JH. Synaptopodin is dispensable for normal podocyte homeostasis but is protective in the context of acute podocyte injury.
J Am Soc Nephrol 2020;31:2815ŌĆō2832.



42. Ashraf S, Gee HY, Woerner S, et al. ADCK4 mutations promote steroid-resistant nephrotic syndrome through CoQ10 biosynthesis disruption.
J Clin Invest 2013;123:5179ŌĆō5189.



43. Widmeier E, Yu S, Nag A, et al. ADCK4 deficiency destabilizes the coenzyme Q Complex, which is rescued by 2,4-dihydroxybenzoic acid treatment.
J Am Soc Nephrol 2020;31:1191ŌĆō1211.



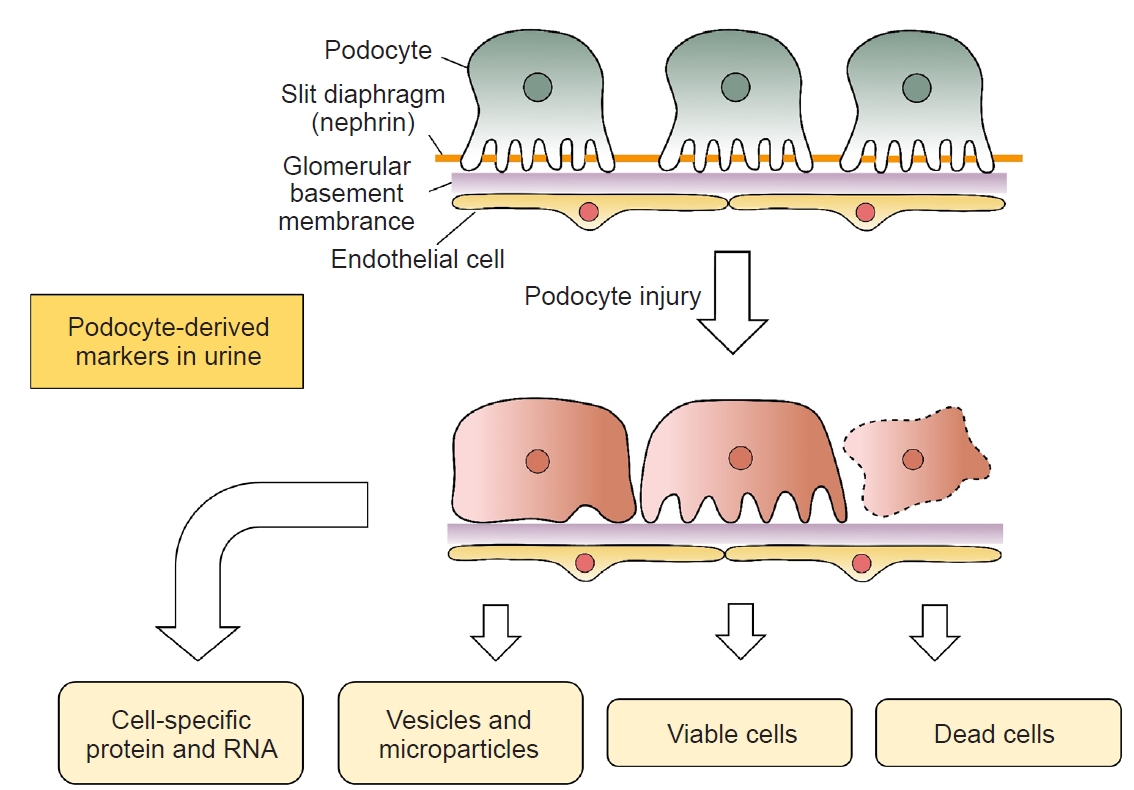
44. Vogelmann SU, Nelson WJ, Myers BD, Lemley KV. Urinary excretion of viable podocytes in health and renal disease.
Am J Physiol Renal Physiol 2003;285:F40ŌĆōF48.



45. Kriz W, Lemley KV. A potential role for mechanical forces in the detachment of podocytes and the progression of CKD.
J Am Soc Nephrol 2015;26:258ŌĆō269.



46. Hara M, Yamamoto T, Yanagihara T, et al. Urinary excretion of podocalyxin indicates glomerular epithelial cell injuries in glomerulonephritis.
Nephron 1995;69:397ŌĆō403.



47. Garovic VD, Craici IM, Wagner SJ, et al. Mass spectrometry as a novel method for detection of podocyturia in pre-eclampsia.
Nephrol Dial Transplant 2013;28:1555ŌĆō1561.



48. Shankland SJ, Pippin JW, Reiser J, Mundel P. Podocytes in culture: past, present, and future.
Kidney Int 2007;72:26ŌĆō36.


49. van der Pol E, B├Čing AN, Harrison P, Sturk A, Nieuwland R. Classification, functions, and clinical relevance of extracellular vesicles.
Pharmacol Rev 2012;64:676ŌĆō705.


50. Zhou H, Yuen PS, Pisitkun T, et al. Collection, storage, preservation, and normalization of human urinary exosomes for biomarker discovery.
Kidney Int 2006;69:1471ŌĆō1476.



51. Hara M, Yanagihara T, Kihara I, Higashi K, Fujimoto K, Kajita T. Apical cell membranes are shed into urine from injured podocytes: a novel phenomenon of podocyte injury.
J Am Soc Nephrol 2005;16:408ŌĆō416.

52. Sharma K. Tell-tale signs of perturbed podocytes.
J Am Soc Nephrol 2014;25:1367ŌĆō1369.



53. Burger D, Thibodeau JF, Holterman CE, Burns KD, Touyz RM, Kennedy CR. Urinary podocyte microparticles identify prealbuminuric diabetic glomerular injury.
J Am Soc Nephrol 2014;25:1401ŌĆō1407.



54. Fukuda A, Minakawa A, Sato Y, et al. Urinary podocyte and TGF-╬▓1 mRNA as markers for disease activity and progression in anti-glomerular basement membrane nephritis.
Nephrol Dial Transplant 2017;32:1818ŌĆō1830.



55. Garg P. A review of podocyte biology.
Am J Nephrol 2018;47 Suppl 1:3ŌĆō13.



57. Son GH, Kwon JY, Lee S, et al. Comparison of serum and urinary nephrin levels between normal pregnancies and severe preeclampsia.
Eur J Obstet Gynecol Reprod Biol 2013;166:139ŌĆō144.


58. Palacios de Franco Y, Velazquez K, Segovia N, et al. Urinary podocalyxin as a marker of preeclampsia in a Hispanic population.
Int J Physiol Pathophysiol Pharmacol 2014;6:115ŌĆō124.


59. Kelder TP, Penning ME, Uh HW, et al. Quantitative polymerase chain reaction-based analysis of podocyturia is a feasible diagnostic tool in preeclampsia.
Hypertension 2012;60:1538ŌĆō1544.


60. Fukuda A, Wickman LT, Venkatareddy MP, et al. Urine podocin: nephrin mRNA ratio (PNR) as a podocyte stress biomarker.
Nephrol Dial Transplant 2012;27:4079ŌĆō4087.



61. Naik AS, Le D, Aqeel J, et al. Podocyte stress and detachment measured in urine are related to mean arterial pressure in healthy humans.
Kidney Int 2020;98:699ŌĆō707.



62. Sato Y, Wharram BL, Lee SK, et al. Urine podocyte mRNAs mark progression of renal disease.
J Am Soc Nephrol 2009;20:1041ŌĆō1052.



63. Trionfini P, Benigni A. MicroRNAs as master regulators of glomerular function in health and disease.
J Am Soc Nephrol 2017;28:1686ŌĆō1696.



64. Wang G, Szeto CC. Methods of microRNA quantification in urinary sediment.
Methods Mol Biol 2013;1024:211ŌĆō220.


65. Ishii H, Kaneko S, Yanai K, et al. MicroRNAs in podocyte injury in diabetic nephropathy.
Front Genet 2020;11:993.



66. Ho J, Ng KH, Rosen S, Dostal A, Gregory RI, Kreidberg JA. Podocyte-specific loss of functional microRNAs leads to rapid glomerular and tubular injury.
J Am Soc Nephrol 2008;19:2069ŌĆō2075.



67. Milas O, Gadalean F, Vlad A, et al. Deregulated profiles of urinary microRNAs may explain podocyte injury and proximal tubule dysfunction in normoalbuminuric patients with type 2 diabetes mellitus.
J Investig Med 2018;66:747ŌĆō754.



68. Li TS, Chen L, Wang SC, et al. Magnesium isoglycyrrhizinate ameliorates fructose-induced podocyte apoptosis through downregulation of miR-193a to increase WT1.
Biochem Pharmacol 2019;166:139ŌĆō152.


69. Ichii O, Otsuka-Kanazawa S, Horino T, et al. Decreased miR-26a expression correlates with the progression of podocyte injury in autoimmune glomerulonephritis.
PLoS One 2014;9:e110383.



72. Wang F, Gao X, Zhang R, Zhao P, Sun Y, Li C. LncRNA TUG1 ameliorates diabetic nephropathy by inhibiting miR-21 to promote TIMP3-expression.
Int J Clin Exp Pathol 2019;12:717ŌĆō729.


73. Koga K, Yokoi H, Mori K, et al. MicroRNA-26a inhibits TGF-╬▓-induced extracellular matrix protein expression in podocytes by targeting CTGF and is downregulated in diabetic nephropathy.
Diabetologia 2015;58:2169ŌĆō2180.



74. Zhao B, Li H, Liu J, et al. MicroRNA-23b targets Ras GTPase-activating protein SH3 domain-binding protein 2 to alleviate fibrosis and albuminuria in diabetic nephropathy.
J Am Soc Nephrol 2016;27:2597ŌĆō2608.



75. Long J, Wang Y, Wang W, Chang BH, Danesh FR. MicroRNA-29c is a signature microRNA under high glucose conditions that targets Sprouty homolog 1, and its in vivo knockdown prevents progression of diabetic nephropathy.
J Biol Chem 2011;286:11837ŌĆō11848.



76. Ramezani A, Devaney JM, Cohen S, et al. Circulating and urinary microRNA profile in focal segmental glomerulosclerosis: a pilot study.
Eur J Clin Invest 2015;45:394ŌĆō404.


77. Kamel KS, Halperin ML. Use of urine electrolytes and urine osmolality in the clinical diagnosis of fluid, electrolytes, and acid-base disorders.
Kidney Int Rep 2021;6:1211ŌĆō1224.



78. Rossing P, Caramori ML, Chan JC, et al. Executive summary of the KDIGO 2022 clinical practice guideline for diabetes management in chronic kidney disease: an update based on rapidly emerging new evidence.
Kidney Int 2022;102:990ŌĆō999.



80. Kostovska I, Tosheska-Trajkovska K, Topuzovska S, et al. Urinary nephrin is earlier, more sensitive and specific marker of diabetic nephropathy than microalbuminuria.
J Med Biochem 2020;39:83ŌĆō90.



81. Hara M, Yamagata K, Tomino Y, et al. Urinary podocalyxin is an early marker for podocyte injury in patients with diabetes: establishment of a highly sensitive ELISA to detect urinary podocalyxin.
Diabetologia 2012;55:2913ŌĆō2919.



82. Shoji M, Kobayashi K, Takemoto M, Sato Y, Yokote K. Urinary podocalyxin levels were associated with urinary albumin levels among patients with diabetes.
Biomarkers 2016;21:164ŌĆō167.


83. Liang X, Wang P, Chen B, et al. Glycogen synthase kinase 3╬▓ hyperactivity in urinary exfoliated cells predicts progression of diabetic kidney disease.
Kidney Int 2020;97:175ŌĆō192.


85. Wang G, Lai FM, Lai KB, Chow KM, Li KT, Szeto CC. Messenger RNA expression of podocyte-associated molecules in the urinary sediment of patients with diabetic nephropathy.
Nephron Clin Pract 2007;106:c169ŌĆōc179.



89. Wickman L, Afshinnia F, Wang SQ, et al. Urine podocyte mRNAs, proteinuria, and progression in human glomerular diseases.
J Am Soc Nephrol 2013;24:2081ŌĆō2095.



90. Zeng L, Fung WW, Chan GC, Ng JK, Chow KM, Szeto CC. Urinary and kidney podocalyxin and podocin levels in diabetic kidney disease: a kidney biopsy study.
Kidney Med 2023;5:100569.


92. Mamdouh S, Sherif H, Romeih M, Elesaily K. Urine micro-RNA signature as a potential non-invasive diagnostic biomarker in bladder cancer.
Asian Pac J Cancer Prev 2023;24:121ŌĆō131.



93. Baumgart S, Meschkat P, Edelmann P, et al. MicroRNAs in tumor samples and urinary extracellular vesicles as a putative diagnostic tool for muscle-invasive bladder cancer.
J Cancer Res Clin Oncol 2019;145:2725ŌĆō2736.



94. Tepus M, Tonoli E, Verderio EAM. Molecular profiling of urinary extracellular vesicles in chronic kidney disease and renal fibrosis.
Front Pharmacol 2022;13:1041327.


95. Mighty J, Rubio-Navarro A, Shi C, et al. Extracellular vesicles of human diabetic retinopathy retinal tissue and urine of diabetic retinopathy patients are enriched for the junction plakoglo bin protein.
Front Endocrinol (Lausanne) 2022;13:1077644.


96. Barreiro K, Dwivedi OP, Rannikko A, et al. Capturing the kidney transcriptome by urinary extracellular vesicles-from pre-analytical obstacles to biomarker research.
Genes (Basel) 2023;14:1415.









 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print















