Idiopathic retroperitoneal fibrosis associated with Hashimoto's thyroiditis in a patient with a single functioning kidney
Article information
Abstract
Retroperitoneal fibrosis (RPF) is a rare disease characterized by the presence of fibroinflammatory tissue around the abdominal aorta and ureteral entrapment in most cases. Idiopathic RPF is frequently reported in association with autoimmune diseases; however, there have been few reports of idiopathic RPF associated with Hashimoto's thyroiditis. Here, we report a case of idiopathic RPF with Hashimoto's thyroiditis in a patient with a single functioning kidney, which was successfully treated by corticosteroid therapy and transient intraureteral stent insertion with a double-J catheter.
Introduction
Retroperitoneal fibrosis (RPF) is a rare disease with an unclear etiology and is characterized by chronic nonspecific inflammation of the retroperitoneum. The hallmark of this disease and its main complication is ureteral entrapment, which is often silent and progressive [1], [2]. Several studies have noted that patients with idiopathic RPF are more likely to suffer from other autoimmune diseases such as autoimmune pancreatitis or Riedel's thyroiditis [3], [4]. However, there have been few reports of cases of idiopathic RPF associated with Hashimoto's thyroiditis, particularly in patients with a single functioning kidney. In this report, we describe the case of idiopathic RPF in a Hashimoto's thyroiditis patient with a single functioning kidney, which was successfully with corticosteroid therapy and transient intraureteral stent insertion using a double-J catheter.
Case report
A 73-year-old Korean woman presented to our outpatient clinic with a complaint of right flank pain for the past 2 days. She had a 5-year history of hypertension and was taking a calcium channel blocker and a beta-blocker. On admission, her blood pressure was 150/80 mmHg. Her lower extremities showed grade 1 pretibial pitting edema.
Chest radiograph images showed no abnormalities. Both kidneys showed elevated renal parenchymal echogenicity and small size (right kidney, 8.5 ×4.4 cm; left kidney, 6.5 ×3.1 cm; Fig. 1). In addition, her right kidney showed hydronephrosis. Her blood urea nitrogen and serum creatinine concentrations were 10.4 mmol/L (reference value: 2.8–7.1 mmol/L) and 282.9 µmol/L (53-106 µmol/L), respectively; 2 weeks earlier, her serum creatinine concentration had been 150.3 µmol/L. The patient's urinary protein excretion was 0.4 g/day. Her hemoglobin concentration was 82 g/L (140-175 g/L) and her serum protein level was 66 g/L (60-80 g/L). The serum concentration of C-reactive protein was 78.6 nmol/L (0.76-28.5 nmol/L). Her thyrotropin, triiodothyronine, and free thyroxine levels were 128.42 µIU/mL (0.3–4.0 µIU/mL), 0.01 nmol/L (0.92–2.76 nmol/L), and 5.53 pmol/L (12–30 pmol/L), respectively. Her anti-thyroglobulin antibody and anti-microsomal antibody titers were both high at 1,462.54 IU/mL (0–60 IU/mL) and 4,658.12 IU/mL (0–60 IU/mL), respectively.
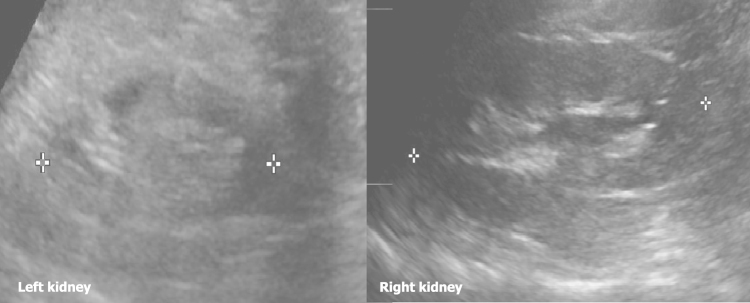
Renal ultrasonography. Both kidneys show increased renal parenchymal echogenicity and decreased size: right kidney, 8.5 cm×4.4 cm; left kidney, 6.5 cm×3.1 cm.
Hydronephrosis was suspected and the patient underwent an abdominal computed tomography (CT) scan. The scan revealed a diffuse infiltrating mass extending from the lower pole of the right kidney to the level of the aortic bifurcation and right ureteral obstruction, as well as moderate hydronephrotic and hydroureteric changes on both sides (Fig. 2A). We diagnosed the patient with postrenal acute renal failure and underlying chronic kidney disease and performed an ultrasonography-guided percutaneous nephrostomy. After percutaneous nephrostomy and consecutive double-J stent insertion, her right flank pain resolved and her serum creatinine level improved to 114.4 µmol/L. She underwent Tc-99m diethylenetriamine pentaacetate renography, which revealed the function of the left kidney to be impaired relative to that of the right (5.8% vs. 94.2%; Fig. 3). To evaluate the underlying cause of her RPF, the patient underwent positron emission tomography combined with CT, which yielded no additional specific finding except for low attenuation with hypermetabolic activity in both lobes of the thyroid gland.
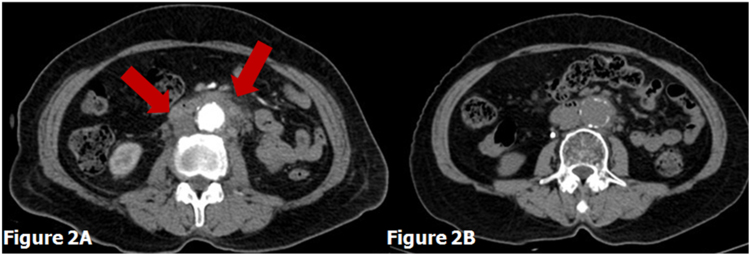
Computed Tomography before and after treatment. (A) Abdominal computed tomography (CT) scan results revealed a diffuse infiltrating mass extending from the lower pole of the kidney to the aortic bifurcation level, as well as ureteral obstruction and moderate hydronephrotic and hydroureteric changes on both sides (arrows). (B) The retroperitoneal mass almost disappeared at the follow-up abdominal CT scan.
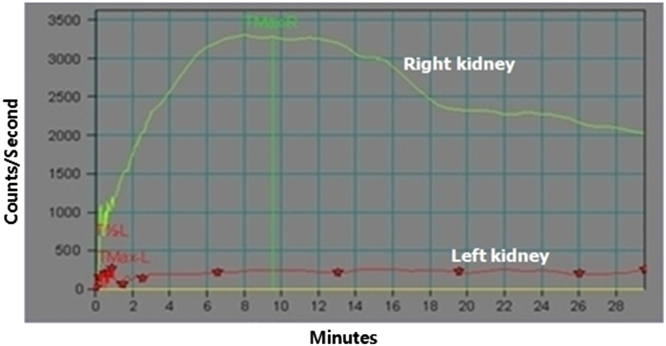
Renography with Tc-99m diethylenetriamine pentaacetate. The function of left kidney was impaired in comparison with the right kidney (5.8% vs. 94.2%).
Oral administration of prednisolone (0.5 mg/kg) and levothyroxine (0.1 mg/day) was initiated on Day 18 of hospitalization on the basis of the presumptive diagnosis of RPF associated with Hashimoto's thyroiditis. After 1 month of steroid and levothyroxine therapy, her thyroid function had recovered to normal levels and a follow-up abdominal CT scan revealed that the retroperitoneal mass almost disappeared (Fig. 2B). The double-J catheter was removed 3 months later. The dose of corticosteroid was tapered to 6 mg/day during the next 6 months. At the 9-month follow-up visit, the patient's serum creatinine level was 106.8 µmol/L.
Discussion
We herein presented a case of idiopathic RPF associated with Hashimoto's thyroiditis in a patient with a single functioning kidney. The patient's serum creatinine level returned to the baseline level after ureteral decompression and corticosteroid treatment. Her thyroid function also became normal after treatment with levothyroxine.
Although idiopathic RPF has been reported in association with autoimmune disorders, there have been few reports of idiopathic RPF associated with autoimmune thyroiditis [3], [4], [5]. Most reports of idiopathic RPF in combination with chronic thyroiditis involved cases of Riedel's thyroiditis, in which the thyroid gland is replaced by fibrous tissue [5], [6]. A previous study reported that 30% of patients with Riedel's thyroiditis subsequently developed idiopathic RPF [6]. In our case, the patient had severe hypothyroidism and high serum concentrations of autoimmune antibodies, which together were suggestive of Hashimoto's thyroiditis [7]. Levothyroxine treatment had restored her thyroid function to normal, as noted during her 1-month follow-up examination.
The patient's renogram showed impaired function of the atrophied left kidney, which was attributed to RPF. Moreover, her serum creatinine increased rapidly from 150.3 to 282.9 µmol/L in just 2 weeks. Patients with an atrophied kidney may be predisposed to develop renal dysfunction rapidly if aggravated idiopathic RPF causes hydronephrosis of the functional contralateral kidney. Our patient's renal function improved after percutaneous nephrostomy. Therefore, percutaneous nephrostomy and consecutive double-J stent insertion should be considered in idiopathic RPF patients with a single functioning kidney.
Glucocorticoid administration with or without ureteral decompression is generally considered the standard treatment for idiopathic RPF [1], [8]. However, there is no guideline concerning the optimal dose of steroid or duration of treatment for the management of idiopathic RPF. Vaglio et al [9] reported that prednisone is more effective than tamoxifen in preventing the recurrence of RPF; in their study, patients received 1 mg/kg of prednisone daily for 1 month. However, Moulik et al [10] reported the successful treatment of a case of Riedel's thyroiditis and idiopathic RPF with a modest dose of prednisolone (30 mg/day). Therefore, we decided to start treatment with a dose of 30 mg prednisone/day because of the high incidence of steroid-induced complications [11]. Our patient recovered without experiencing any side effects of the corticosteroid.
In summary, we successfully treated idiopathic RPF in association with Hashimoto's thyroiditis in a patient with a single functioning kidney by corticosteroid therapy and transient intraureteral stent insertion with a double-J catheter.
Conflict of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.