1. Jha V, Garcia-Garcia G, Iseki K, et al. Chronic kidney disease: global dimension and perspectives.
Lancet 2013;382:260–272.


2. Chen YC, Cheng CY, Liu CT, et al. Combined protective effects of oligo-fucoidan, fucoxanthin, and L-carnitine on the kidneys of chronic kidney disease mice.
Eur J Pharmacol 2021;892:173708.


4. Chevalier RL, Forbes MS, Thornhill BA. Ureteral obstruction as a model of renal interstitial fibrosis and obstructive nephropathy.
Kidney Int 2009;75:1145–1152.


5. Martínez-Klimova E, Aparicio-Trejo OE, Tapia E, Pedraza-Chaverri J. Unilateral ureteral obstruction as a model to investigate fibrosis-attenuating treatments.
Biomolecules 2019;9:141.



6. Mack M, Yanagita M. Origin of myofibroblasts and cellular events triggering fibrosis.
Kidney Int 2015;87:297–307.


7. Shu DY, Lovicu FJ. Myofibroblast transdifferentiation: the dark force in ocular wound healing and fibrosis.
Prog Retin Eye Res 2017;60:44–65.



8. da Silva Oliveira GL, de Freitas RM. Diminazene aceturate: an antiparasitic drug of antiquity: advances in pharmacology & therapeutics.
Pharmacol Res 2015;102:138–157.


9. Qaradakhi T, Gadanec LK, McSweeney KR, et al. The potential actions of angiotensin-converting enzyme II (ACE2) activator diminazene aceturate (DIZE) in various diseases.
Clin Exp Pharmacol Physiol 2020;47:751–758.



11. Chappell MC, Al Zayadneh EM. Angiotensin-(1-7) and the regulation of anti-fibrotic signaling pathways.
J Cell Signal 2017;2:134.



12. Kim CS, Kim IJ, Bae EH, Ma SK, Lee J, Kim SW. Angiotensin-(1-7) attenuates kidney injury due to obstructive nephropathy in rats.
PLoS One 2015;10:e0142664.



13. Rago F, Melo EM, Kraemer L, et al. Effect of preventive or therapeutic treatment with angiotensin 1-7 in a model of bleomycin-induced lung fibrosis in mice.
J Leukoc Biol 2019;106:677–686.



14. Cai SM, Yang RQ, Li Y, et al. Angiotensin-(1-7) improves liver fibrosis by regulating the NLRP3 inflammasome via redox balance modulation.
Antioxid Redox Signal 2016;24:795–812.


15. Haber PK, Ye M, Wysocki J, Maier C, Haque SK, Batlle D. Angiotensin-converting enzyme 2-independent action of presumed angiotensin-converting enzyme 2 activators: studies in vivo, ex vivo, and in vitro.
Hypertension 2014;63:774–782.


17. Velkoska E, Patel SK, Griggs K, Burrell LM. Diminazene aceturate improves cardiac fibrosis and diastolic dysfunction in rats with kidney disease.
PLoS One 2016;11:e0161760.



18. Han SJ, Noh MR, Jung JM, et al. Hydrogen sulfide-producing cystathionine γ-lyase is critical in the progression of kidney fibrosis.
Free Radic Biol Med 2017;112:423–432.


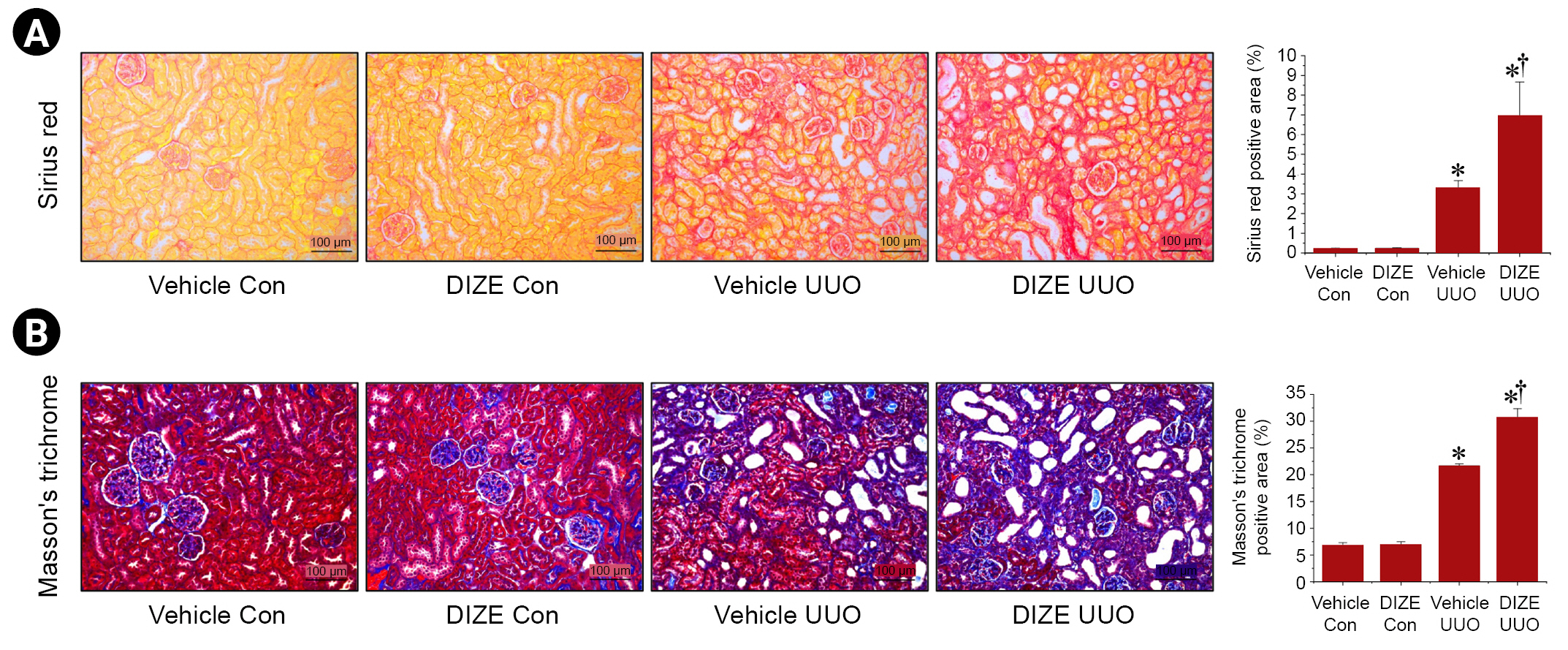
20. Costa GM, Araujo SL, Xavier FA, et al. Picrosirius red and masson’s trichrome staining techniques as tools for detection of collagen fibers in the skin of dogs with endocrine dermatopathologies.
Ciênc Anim Bras 2019;20:e-55398.

21. Crowe AR, Yue W. Semi-quantitative determination of protein expression using immunohistochemistry staining and analysis: an integrated protocol.
Bio Protoc 2019;9:e3465.



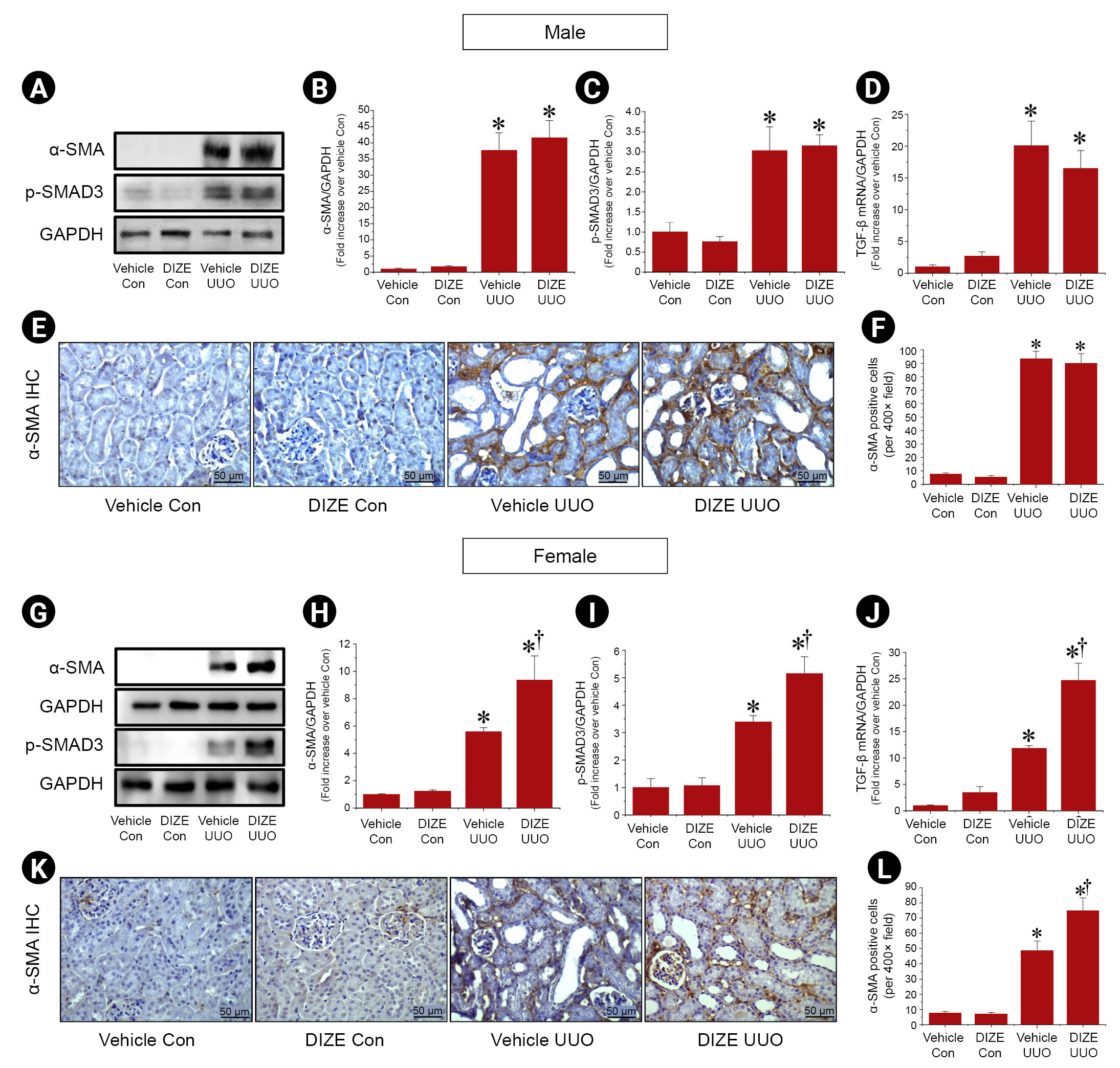
23. Meng XM, Tang PM, Li J, Lan HY. TGF-β/Smad signaling in renal fibrosis.
Front Physiol 2015;6:82.



24. Liu Z, Huang XR, Chen HY, Penninger JM, Lan HY. Loss of angiotensin-converting enzyme 2 enhances TGF-β/Smad-mediated renal fibrosis and NF-κB-driven renal inflammation in a mouse model of obstructive nephropathy.
Lab Invest 2012;92:650–661.



25. Feng Y, Liang Y, Zhu X, et al. The signaling protein Wnt5a promotes TGFβ1-mediated macrophage polarization and kidney fibrosis by inducing the transcriptional regulators Yap/Taz.
J Biol Chem 2018;293:19290–19302.



26. Stachowicz A, Wiśniewska A, Kuś K, et al. Diminazene aceturate stabilizes atherosclerotic plaque and attenuates hepatic steatosis in apoE-knockout mice by influencing macrophages polarization and taurine biosynthesis.
Int J Mol Sci 2021;22:5861.



27. Xu ZJ, Gu Y, Wang CZ, et al. The M2 macrophage marker CD206: a novel prognostic indicator for acute myeloid leukemia.
Oncoimmunology 2019;9:1683347.



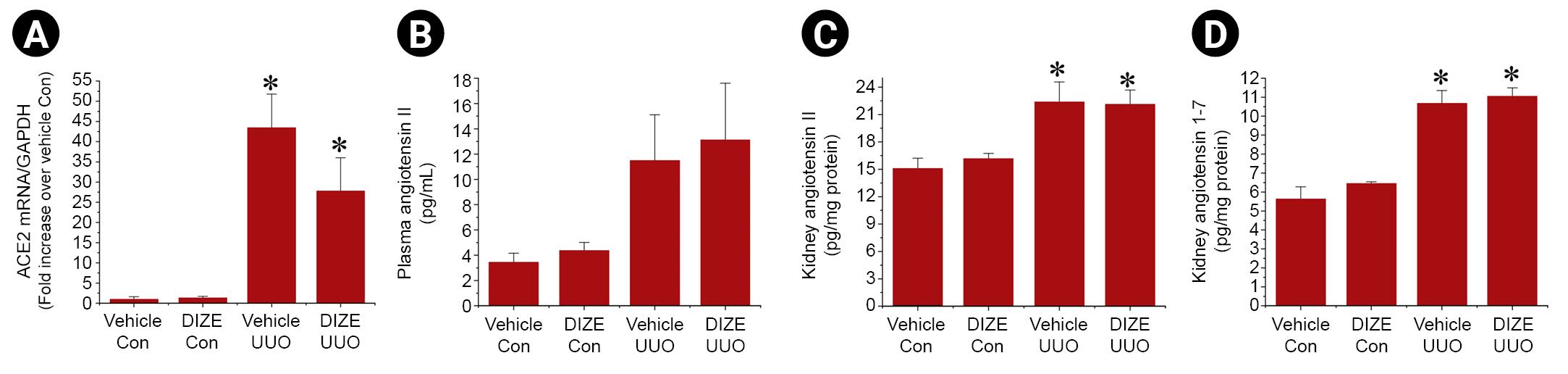
28. Zimmerman DL, Zimpelmann J, Xiao F, Gutsol A, Touyz R, Burns KD. The effect of angiotensin-(1-7) in mouse unilateral ureteral obstruction.
Am J Pathol 2015;185:729–740.


30. Pendergrass KD, Pirro NT, Westwood BM, Ferrario CM, Brosnihan KB, Chappell MC. Sex differences in circulating and renal angiotensins of hypertensive mRen(2).Lewis but not normotensive lewis rats.
Am J Physiol Heart Circ Physiol 2008;295:H10–H20.


31. Soro-Paavonen A, Gordin D, Forsblom C, et al. Circulating ACE2 activity is increased in patients with type 1 diabetes and vascular complications.
J Hypertens 2012;30:375–383.


32. Shapouri-Moghaddam A, Mohammadian S, Vazini H, et al. Macrophage plasticity, polarization, and function in health and disease.
J Cell Physiol 2018;233:6425–6440.


33. Cao Q, Harris DC, Wang Y. Macrophages in kidney injury, inflammation, and fibrosis.
Physiology (Bethesda) 2015;30:183–194.


34. Zhu L, Fu X, Chen X, Han X, Dong P. M2 macrophages induce EMT through the TGF-β/Smad2 signaling pathway.
Cell Biol Int 2017;41:960–968.












 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print















