1. Kaesler N, Babler A, Floege J, Kramann R. Cardiac remodeling in chronic kidney disease.
Toxins (Basel) 2020;12:161.



2. GBD Chronic Kidney Disease Collaboration. Global, regional, and national burden of chronic kidney disease, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017.
Lancet 2020;395:709–733.


3. Shamseddin MK, Parfrey PS. Sudden cardiac death in chronic kidney disease: epidemiology and prevention.
Nat Rev Nephrol 2011;7:145–154.



4. Ravarotto V, Simioni F, Pagnin E, Davis PA, Calò LA. Oxidative stress - chronic kidney disease - cardiovascular disease: a vicious circle.
Life Sci 2018;210:125–131.


5. Roehm B, Weiner DE. Blood pressure targets and kidney and cardiovascular disease: same data but discordant guidelines.
Curr Opin Nephrol Hypertens 2019;28:245–250.


6. Zewinger S, Kleber ME, Rohrer L, et al. Symmetric dimethylarginine, high-density lipoproteins and cardiovascular disease.
Eur Heart J 2017;38:1597–1607.


7. Chen SC, Hung CC, Kuo MC, et al. Association of dyslipidemia with renal outcomes in chronic kidney disease.
PloS One 2013;8:e55643.



8. Schlesinger S, Neuenschwander M, Barbaresko J, et al. Prediabetes and risk of mortality, diabetes-related complications and comorbidities: umbrella review of meta-analyses of prospective studies.
Diabetologia 2022;65:275–285.



9. Jankowski J, Floege J, Fliser D, Böhm M, Marx N. Cardiovascular disease in chronic kidney disease: pathophysiological insights and therapeutic options.
Circulation 2021;143:1157–1172.



11. Koenigsberger M, Sauser R, Bény JL, Meister JJ. Role of the endothelium on arterial vasomotion.
Biophys J 2005;88:3845–3854.



12. Sata Y, Burke SL, Gueguen C, et al. Contribution of the renal nerves to hypertension in a rabbit model of chronic kidney disease.
Hypertension 2020;76:1470–1479.


13. Garimella PS, Katz R, Waikar SS, et al. Kidney tubulointerstitial fibrosis and tubular secretion.
Am J Kidney Dis 2022;79:709–716.


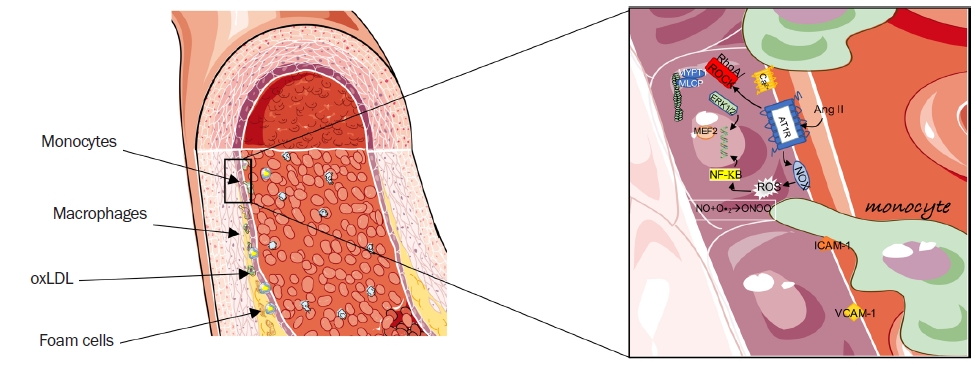
15. Poznyak AV, Bharadwaj D, Prasad G, Grechko AV, Sazonova MA, Orekhov AN. Renin-angiotensin system in pathogenesis of atherosclerosis and treatment of CVD.
Int J Mol Sci 2021;22:6702.



16. Moriya J. Critical roles of inflammation in atherosclerosis.
J Cardiol 2019;73:22–27.


17. Van Tits L, De Graaf J, Hak-Lemmers H, et al. Increased levels of low-density lipoprotein oxidation in patients with familial hypercholesterolemia and in end-stage renal disease patients on hemodialysis.
Lab Invest 2003;83:13–21.


18. Zuo Y, Yancey P, Castro I, et al. Renal dysfunction potentiates foam cell formation by repressing ABCA1.
Arterioscler Thromb Vasc Biol 2009;29:1277–1282.



20. Seccia TM, Rigato M, Ravarotto V, Calò LA. ROCK (RhoA/Rho Kinase) in cardiovascular-renal pathophysiology: a review of new advancements.
J Clin Med 2020;9:1328.



21. Kloc M, Uosef A, Kubiak JZ, Ghobrial RM. Role of macrophages and RhoA pathway in atherosclerosis.
Int J Mol Sci 2020;22:216.



22. Hohensinner PJ, Baumgartner J, Kral-Pointner JB, et al. PAI-1 (plasminogen activator inhibitor-1) expression renders alternatively activated human macrophages proteolytically quiescent.
Arterioscler Thromb Vasc Biol 2017;37:1913–1922.



23. Sell DR, Monnier VM. Molecular basis of arterial stiffening: role of glycation: a mini-review.
Gerontology 2012;58:227–237.



24. Qian J, Zhong J, Liu S, et al. α-Klotho, plasma asymmetric dimethylarginine, and kidney disease progression.
Kidney Med 2021;3:984–991.



25. Kuro-o M, Matsumura Y, Aizawa H, et al. Mutation of the mouse klotho gene leads to a syndrome resembling ageing.
Nature 1997;390:45–51.



27. Stevens KK, Denby L, Patel RK, et al. Deleterious effects of phosphate on vascular and endothelial function via disruption to the nitric oxide pathway.
Nephrol Dial Transplant 2017;32:1617–1627.


28. Yeung CK, Shen DD, Thummel KE, Himmelfarb J. Effects of chronic kidney disease and uremia on hepatic drug metabolism and transport.
Kidney Int 2014;85:522–528.


29. Seccia TM, Caroccia B, Piazza M, Rossi GP. The key role of epithelial to mesenchymal transition (EMT) in hypertensive kidney disease.
Int J Mol Sci 2019;20:3567.



30. Kidney Disease: Improving Global Outcomes (KDIGO) Blood Pressure Work Group. KDIGO 2021 clinical practice guideline for the management of blood pressure in chronic kidney disease.
Kidney Int 2021;99(3S):S1–S87.


31. Gansevoort RT, Correa-Rotter R, Hemmelgarn BR, et al. Chronic kidney disease and cardiovascular risk: epidemiology, mechanisms, and prevention.
Lancet 2013;382:339–352.


32. van der Velde M, Matsushita K, Coresh J, et al. Lower estimated glomerular filtration rate and higher albuminuria are associated with all-cause and cardiovascular mortality: a collaborative meta-analysis of high-risk population cohorts.
Kidney Int 2011;79:1341–1352.


33. Chronic Kidney Disease Prognosis Consortium, Matsushita K, van der Velde M, et al. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis.
Lancet 2010;375:2073–2081.



34. Foudi N, Palayer M, Briet M, Garnier AS. Arterial remodelling in chronic kidney disease: impact of uraemic toxins and new pharmacological approaches.
J Clin Med 2021;10:3803.



35. Vanholder R, Pletinck A, Schepers E, Glorieux G. Biochemical and clinical impact of organic uremic retention solutes: a comprehensive update.
Toxins (Basel) 2018;10:33.



36. Méndez-Barbero N, Gutiérrez-Muñoz C, Blanco-Colio LM. Cellular crosstalk between endothelial and smooth muscle cells in vascular wall remodeling.
Int J Mol Sci 2021;22:7284.



37. Chitalia N, Ross L, Krishnamoorthy M, et al. Neointimal hyperplasia and calcification in medium sized arteries in adult patients with chronic kidney disease.
Semin Dial 2015;28:E35–E40.


38. Lacolley P, Regnault V, Segers P, Laurent S. Vascular smooth muscle cells and arterial stiffening: relevance in development, aging, and disease.
Physiol Rev 2017;97:1555–1617.


39. Seccia TM, Caroccia B, Calò LA. Hypertensive nephropathy: moving from classic to emerging pathogenetic mechanisms.
J Hypertens 2017;35:205–212.


40. Pengo MF, Ioratti D, Bisogni V, et al. In patients with chronic kidney disease short term blood pressure variability is associated with the presence and severity of sleep disorders.
Kidney Blood Press Res 2017;42:804–815.



41. Sárközy M, Gáspár R, Zvara Á, et al. Chronic kidney disease induces left ventricular overexpression of the pro-hypertrophic microRNA-212.
Sci Rep 2019;9:1302.


42. Sorokin V, Vickneson K, Kofidis T, et al. Role of vascular smooth muscle cell plasticity and interactions in vessel wall inflammation.
Front Immunol 2020;11:599415.



43. Schotten U, Verheule S, Kirchhof P, Goette A. Pathophysiological mechanisms of atrial fibrillation: a translational appraisal.
Physiol Rev 2011;91:265–325.


44. Calò LA, Vertolli U, Pagnin E, et al. Increased rho kinase activity in mononuclear cells of dialysis and stage 3-4 chronic kidney disease patients with left ventricular hypertrophy: cardiovascular risk implications.
Life Sci 2016;148:80–85.


45. Higashi M, Shimokawa H, Hattori T, et al. Long-term inhibition of Rho-kinase suppresses angiotensin II-induced cardiovascular hypertrophy in rats in vivo: effect on endothelial NAD(P)H oxidase system.
Circ Res 2003;93:767–775.

46. Ishimaru K, Ueno H, Kagitani S, Takabayashi D, Takata M, Inoue H. Fasudil attenuates myocardial fibrosis in association with inhibition of monocyte/macrophage infiltration in the heart of DOCA/salt hypertensive rats.
J Cardiovasc Pharmacol 2007;50:187–194.


47. Ravarotto V, Pagnin E, Maiolino G, et al. The blocking of angiotensin II type 1 receptor and RhoA/Rho kinase activity in hypertensive patients: effect of olmesartan medoxomil and implication with cardiovascular-renal remodeling.
J Renin Angiotensin Aldosterone Syst 2015;16:1245–1250.



48. Calo LA, Vertolli U, Davis PA, et al. Molecular biology based assessment of green tea effects on oxidative stress and cardiac remodelling in dialysis patients.
Clin Nutr 2014;33:437–442.


49. Calò LA, Ravarotto V, Bertoldi G, et al. Rho kinase activity, connexin 40, and atrial fibrillation: mechanistic insights from end-stage renal disease on dialysis patients.
J Clin Med 2020;9:165.



50. Chaldoupi SM, Loh P, Hauer RN, de Bakker JM, van Rijen HV. The role of connexin40 in atrial fibrillation.
Cardiovasc Res 2009;84:15–23.


51. Miano JM. Myocardin in biology and disease.
J Biomed Res 2015;29:3–19.

52. Sisson TH, Ajayi IO, Subbotina N, et al. Inhibition of myocardin-related transcription factor/serum response factor signaling decreases lung fibrosis and promotes mesenchymal cell apoptosis.
Am J Pathol 2015;185:969–986.



53. Ku E, Lee BJ, Wei J, Weir MR. Hypertension in CKD: core curriculum 2019.
Am J Kidney Dis 2019;74:120–131.


54. Turner JM, Bauer C, Abramowitz MK, Melamed ML, Hostetter TH. Treatment of chronic kidney disease.
Kidney Int 2012;81:351–362.


55. Hoorn EJ, Walsh SB, McCormick JA, Zietse R, Unwin RJ, Ellison DH. Pathogenesis of calcineurin inhibitor-induced hypertension.
J Nephrol 2012;25:269–275.



56. Calò LA, Ravarotto V, Simioni F, et al. Pathophysiology of post transplant hypertension in kidney transplant: focus on calcineurin inhibitors induced oxidative stress and renal sodium retention and implications with RhoA/Rho kinase pathway.
Kidney Blood Press Res 2017;42:676–685.



57. Sinha AD, Agarwal R. Clinical pharmacology of antihypertensive therapy for the treatment of hypertension in CKD.
Clin J Am Soc Nephrol 2019;14:757–764.


58. Dhondup T, Qian Q. Electrolyte and acid-base disorders in chronic kidney disease and end-stage kidney failure.
Blood Purif 2017;43:179–188.



59. Lin J, Cheng Z, Ding X, Qian Q. Acid-base and electrolyte managements in chronic kidney disease and end-stage renal disease: case-based discussion.
Blood Purif 2018;45:179–186.



60. Lindner G, Burdmann EA, Clase CM, et al. Acute hyperkalemia in the emergency department: a summary from a Kidney Disease: Improving Global Outcomes conference.
Eur J Emerg Med 2020;27:329–337.



61. Beto J, Bhatt N, Gerbeling T, Patel C, Drayer D. Overview of the 2017 KDIGO CKD-MBD update: practice implications for adult hemodialysis patients.
J Ren Nutr 2019;29:2–15.


62. Ravid JD, Kamel MH, Chitalia VC. Uraemic solutes as therapeutic targets in CKD-associated cardiovascular disease.
Nat Rev Nephrol 2021;17:402–416.



64. D’Arrigo G, Baggetta R, Tripepi G, Galli F, Bolignano D. Effects of vitamin E-coated versus conventional membranes in chronic hemodialysis patients: a systematic review and meta-analysis.
Blood Purif 2017;43:101–122.



65. Calò LA, Naso A, D’Angelo A, et al. Molecular biology-based assessment of vitamin E-coated dialyzer effects on oxidative stress, inflammation, and vascular remodeling.
Artif Organs 2011;35:E33–E39.

66. Calò LA, Naso A, Carraro G, et al. Effect of haemodiafiltration with online regeneration of ultrafiltrate on oxidative stress in dialysis patients.
Nephrol Dial Transplant 2007;22:1413–1419.


67. Roumeliotis S, Eleftheriadis T, Liakopoulos V. Is oxidative stress an issue in peritoneal dialysis?
Semin Dial 2019;32:463–466.













 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print















