| Kidney Res Clin Pract > Volume 40(3); 2021 > Article |
|
Abstract
Background
Methods
Results
Notes
Figure┬Ā1.
Kaplan-Meier curves of in-hospital survival among the six groups.

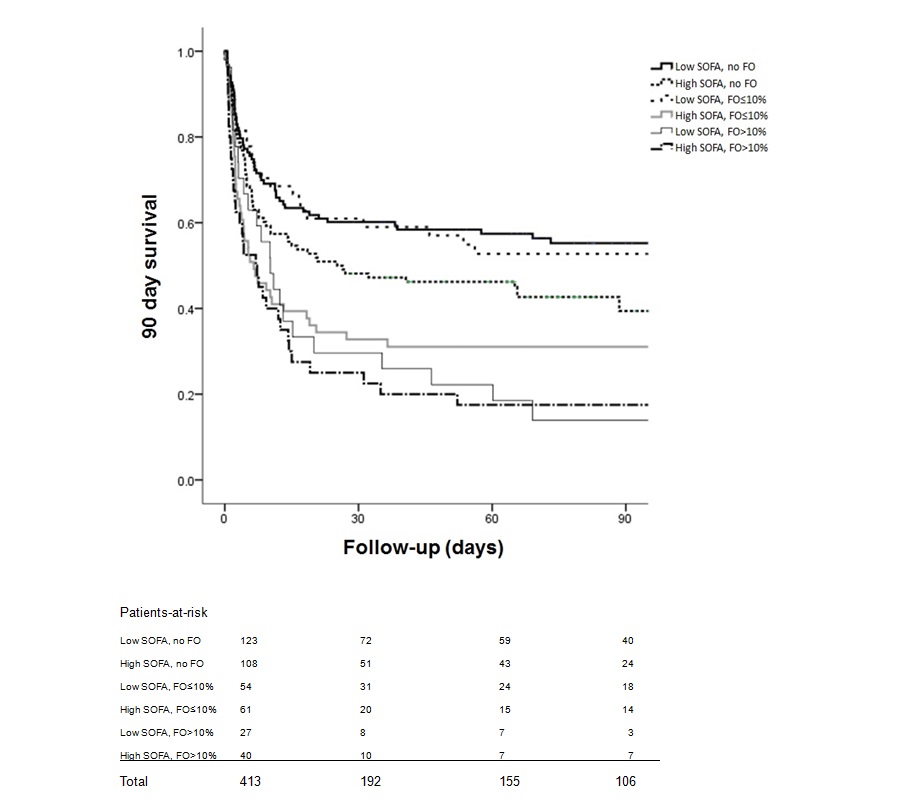
Figure┬Ā2.
Kaplan-Meier curves of 90-day survival among the six groups.
Table┬Ā1.
| Characteristic | Total | Survivor | Non-survivor | p-value |
|---|---|---|---|---|
| No. of patients | 414 | 177 | 237 | |
| Demographic | ||||
| ŌĆāAge (yr) | 66.4 ┬▒ 14.8 | 65.8 ┬▒ 15.3 | 66.8 ┬▒ 14.4 | 0.50 |
| ŌĆāSex | ||||
| ŌĆāŌĆāMale | 282 (68.1) | 120 (67.8) | 162 (68.4) | 0.90 |
| ŌĆāŌĆāFemale | 132 (31.9) | 57 (32.2) | 75 (31.6) | |
| Comorbid disease | ||||
| ŌĆāHypertension | 202 (48.8) | 99 (55.9) | 103 (43.5) | 0.01 |
| ŌĆāDiabetes mellitus | 162 (39.1) | 88 (49.7) | 74 (31.2) | <0.001 |
| ŌĆāMalignancy | 100 (24.2) | 28 (15.8) | 72 (30.4) | 0.001 |
| ŌĆāLiver disease | 63 (15.2) | 23 (13.0) | 40 (16.9) | 0.28 |
| ŌĆāCongestive heart failure | 52 (12.6) | 31 (17.5) | 21 (8.9) | 0.009 |
| ŌĆāMyocardial infarction | 28 (6.8) | 16 (9.0) | 12 (5.1) | 0.11 |
| ŌĆāIschemic heart disease | 21 (5.1) | 10 (5.6) | 11 (4.6) | 0.64 |
| ŌĆāCOPD | 21 (5.1) | 8 (4.5) | 13 (5.5) | 0.66 |
| ŌĆāCerebrovascular accident | 14 (3.4) | 5 (2.8) | 9 (3.8) | 0.59 |
| ŌĆāPeptic ulcer disease | 5 (1.2) | 1 (0.6) | 4 (1.7) | 0.30 |
| MAP (mmHg) | 80.0 ┬▒ 16.8 | 83.2 ┬▒ 17.6 | 77.8 ┬▒ 15.8 | 0.001 |
| Illness severity | ||||
| ŌĆāSOFA scorea | 9.7 ┬▒ 3.6 | 8.9 ┬▒ 3.2 | 10.3 ┬▒ .3.8 | <0.001 |
| ŌĆāVasopressor use | <0.001 | |||
| ŌĆāŌĆāNone | 119 (28.7) | 67 (37.9) | 52 (21.9) | |
| ŌĆāŌĆā1 | 182 (44.0) | 79 (44.6) | 103 (43.5) | |
| ŌĆāŌĆāŌēź2 | 113 (27.3) | 31 (17.5) | 82 (34.6) | |
| ŌĆāUse of mechanical ventilation | 276 (66.7) | 100 (56.5) | 176 (74.3) | <0.001 |
| AKI etiologya | ||||
| ŌĆāPostoperative | 21 (5.1) | 10 (5.6) | 11 (4.6) | 0.71 |
| ŌĆāSeptic | 285 (68.8) | 111 (62.7) | 174 (73.4) | 0.004 |
| ŌĆāCardiogenic | 24 (5.8) | 9 (5.1) | 15 (6.3) | 0.47 |
| ŌĆāOthers | 65 (15.7) | 34 (19.2) | 31 (13.1) | 0.11 |
| Serum creatinine (mg/dL)a | 3.5 ┬▒ 2.5 | 4.3 ┬▒ 3.1 | 2.9 ┬▒ 1.7 | <0.001 |
| Blood pHa | 7.31 ┬▒ 0.13 | 7.33 ┬▒ 0.13 | 7.29 ┬▒ 0.13 | 0.006 |
| UO 24 hours prior to CRRT (L)a | 0.4 ┬▒ 0.6 | 0.4 ┬▒ 0.5 | 0.5 ┬▒ 0.6 | 0.07 |
| Intensive care unit stay (day) | 9.5 ┬▒ 14.8 | 10.8 ┬▒ 17.2 | 8.5 ┬▒ 12.7 | 0.11 |
| Hospital stay (day) | 21.2 ┬▒ 39.3 | 35.8 ┬▒ 54.1 | 10.2 ┬▒ 15.4 | <0.001 |
| CRRT duration (day) | 5.1 ┬▒ 5.6 | 4.6 ┬▒ 4.4 | 5.4 ┬▒ 6.3 | 0.16 |
| Fluid overload | 182 (44.0) | 61 (34.5) | 121 (51.1) | 0.001 |
| Degree of fluid overload | <0.001 | |||
| ŌĆāŌēż10% | 115 (27.8) | 49 (27.7) | 66 (27.8) | |
| ŌĆā>10% | 67 (16.2) | 12 (6.8) | 55 (23.2) |
Data are presented as number only, mean ┬▒ standard deviation for continuous variables, or number (%) for categorical variables.
AKI, acute kidney injury; COPD, chronic obstructive pulmonary disease; CRRT, continuous renal replacement therapy; MAP, mean arterial pressure; SOFA, Sequential Organ Failure Assessment; UO, urine output.
Table┬Ā2.
HRs are expressed per 0.1mg/dL change in creatinine, per 0.1 unit change in pH, per 1 unit change in SOFA score, and presence of fluid overload. Model 1: Cox proportional hazards model of 90-day mortality; model 2: model 1 with adjustments for age and sex; model 3: model 1 with adjustments for age, sex, and the other variables (serum creatinine, blood pH, SOFA score, and fluid overload); model 4: model 1 with adjustments for age, sex, the other variables, diabetes mellitus, hypertension, malignancy, and sepsis.
CI, confidence interval; HR, hazard ratio; SOFA, Sequential Organ Failure Assessment.
Table┬Ā3.
| Fluid overload |
SOFA score < 10 (n = 204) |
SOFA score Ōēź 10 (n = 209) |
||||
|---|---|---|---|---|---|---|
| No (%)a | HR (95% CI) | p-value | No (%)a | HR (95% CI) | p-value | |
| No (n = 231) | 53/70 (43.1) | (Reference) | 63/45 (58.3) | 1.85 (1.10ŌĆō3.12) | 0.02 | |
| Ōēż10% (n = 115) | 24/30 (44.4) | 1.06 (0.56ŌĆō2.01) | 0.87 | 42/19 (68.9) | 2.92 (1.53ŌĆō5.59) | 0.001 |
| >10% (n = 67) | 22/5 (81.5) | 5.81 (2.07ŌĆō16.35) | 0.001 | 33/7 (82.5) | 6.23 (2.56ŌĆō15.17) | <0.001 |
Table┬Ā4.
| Fluid overload |
SOFA score <10 (n = 204) |
SOFA score Ōēź10 (n = 209) |
||||
|---|---|---|---|---|---|---|
| No (%)a | HR (95% CI) | p-value | No (%)a | HR (95% CI) | p-value | |
| No (n = 231) | 54/69 (43.9) | (Reference) | 63/45 (58.3) | 1.79 (1.06ŌĆō3.02) | 0.03 | |
| Ōēż10% (n = 115) | 25/29 (46.3) | 1.10 (0.58ŌĆō2.09) | 0.77 | 43/18 (70.5) | 3.05 (1.59ŌĆō5.88) | 0.001 |
| >10% (n = 67) | 24/3 (88.9) | 10.22 (2.92ŌĆō35.75) | <0.001 | 33/7 (82.5) | 6.02 (2.47ŌĆō14.67) | <0.001 |
References
-
METRICS

- ORCID iDs
-
Kristianne Rachel P. Medina-Liabres

https://orcid.org/0000-0003-1092-1930Jong Cheol Jeong

https://orcid.org/0000-0003-0301-7644Hyung Jung Oh

https://orcid.org/0000-0002-4281-696XJung Nam An

https://orcid.org/0000-0001-5108-1005Jung Pyo Lee

https://orcid.org/0000-0002-4714-1260Dong Ki Kim

https://orcid.org/0000-0002-5195-7852Dong-Ryeol Ryu

https://orcid.org/0000-0002-5309-7606Sejoong Kim

https://orcid.org/0000-0002-7238-9962 - Related articles



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print















