1. Dialysis Therapy (JSDT) . Reports from the Japanese Society for Dialysis Therapy (JSDT). 2014. [in Japanese].
2. Japanese Society of Nephrology (JSN) . Evidence-based Clinical Practice Guideline for CKD 2013. 2013. Tokyo Igakusya; Tokyo: p. ix–xiii. [in Japanese].
3. Katafuchi R.. Differences in etiology and treatment in Japan. In: Tomino Y., Pathogenesis and Treatment in IgA Nephropathy: An International Comparison. 2016. Springer; Tokyo: p. 167–207.
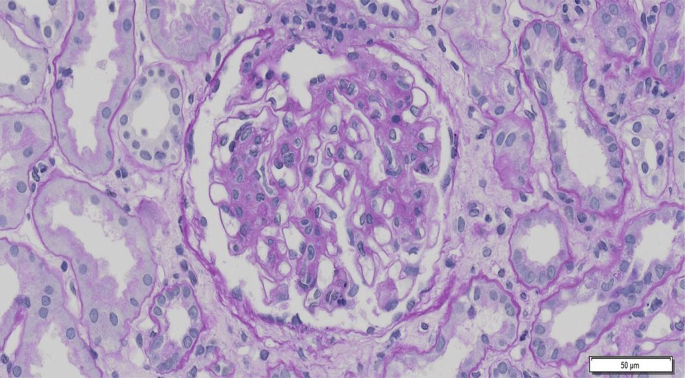
4. Joh K., McNamara K.M.. Differences of histological classification between the Japanese histological grade classification and the Oxford classification. In: Tomino Y., Pathogenesis and Treatment in IgA Nephropathy: An International Comparison. 2016. Springer; Tokyo: p. 69–87.
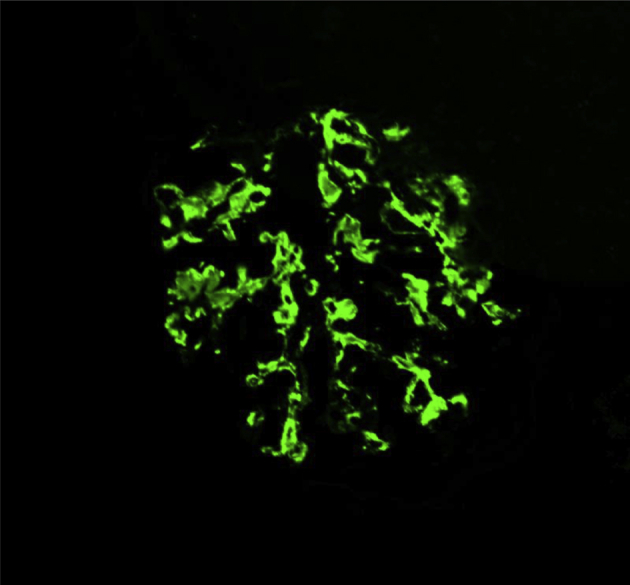
5. Berger J., Hinglais N.. Intercapillary deposits of IgA-IgG. J Urol Nephrol (Paris) 74:1968;694–695.
6. Tomino Y., Suzuki S., Imai H., Saito T., Kawamura T., Yorioka N., Harada T., Yasumoto K., Kida H., Kobayashi Y., Endoh M., Sato H., Saito K.. Measurement of serum IgA and C3 may predict the diagnosis of patients with IgA nephropathy prior to renal biopsy.
J Clin Lab Anal 14:2000;220–223.

7. Maeda A., Gohda T., Funabiki K., Horikoshi S., Shirato I., Tomino Y.. Significance of serum IgA levels and serum IgA/C3 ratio in diagnostic analysis of patients with IgA nephropathy.
J Clin Lab Anal 17:2003;73–76.

8. Novak J., Julian B.A., Tomana M., Mesteck J.. Progress in molecular and genetic studies of IgA nephropathy. J Clin Immunol 21:2001;310–327.
9. Yanagawa H., Suzuki H., Suzuki Y., Kiryluk K., Gharavi A.G., Matsuoka K., Makita Y., Julian B.A., Novak J., Tomino Y.. A panel of serum biomarkers differentiates IgA nephropathy from other renal diseases.
PLoS One 9:2014;e98081



10. Yasutake J., Suzuki Y., Suzuki H., Hiura N., Yanagawa H., Makita Y., Kaneko E., Tomino Y.. Novel lectin-independent approach to detect galactose-deficient IgA1 in IgA nephropathy.
Nephrol Dial Transplant 30:2015;1315–1321.



11. Chan L.Y., Leung J.C., Tsang A.W., Tang S.C., Lai K.N.. Activation of tubular epithelial cells by mesangial-derived TNF-alpha: glomerulotubular communication in IgA nephropathy.
Kidney Int 67:2005;602–612.


12. Sonoda Y., Gohda T., Suzuki Y., Omote K., Ishizaka M., Matsuoka J., Tomino Y.. Circulating TNF receptors 1 and 2 are associated with the severity of renal interstitial fibrosis in IgA nephropathy.
PLoS One 10:2015;e0122212



13. Asao R., Asanuma K., Kodama F., Akiba-Takagi M., Nagai-Hosoe Y., Seki T., Takeda Y., Ohsawa I., Mano S., Matsuoka K., Kurosawa H., Ogasawara S., Hirayama Y., Sekine S., Horikoshi S., Hara M., Tomino Y.. Relationship between levels of urinary podocalyxin, number of podocytes, and histological injury in adult patients with IgA nephropathy.
Clin J Am Soc Nephrol 7:2012;1385–1393.



14. Onda K., Ohsawa I., Ohi H., Tamano M., Mano S., Wakabayashi M., Toki A., Horikoshi S., Fujita T., Tomino Y.. Excretion of complement proteins and its activation marker C5b-9 in IgA nephropathy in relation to renal function.
BMC Nephrol 12:2011;64



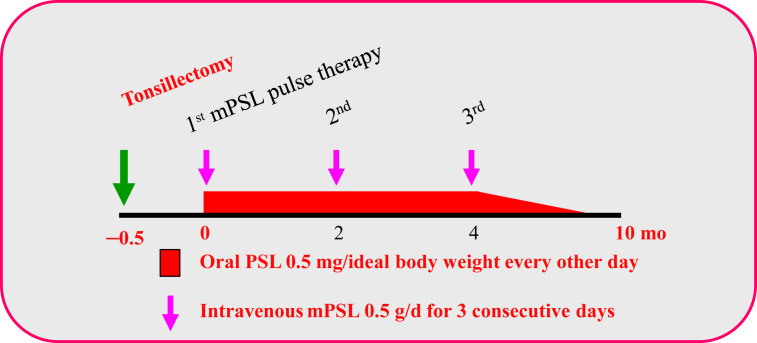
15. Hotta O., Miyazaki M., Furuta T., Tomioka D., Chiba S., Horigome I., Abe K., Taguma Y.. Tonsillectomy and steroid pulse therapy significantly impact on clinical remission in patients with IgA nephropathy.
Am J Kidney Dis 38:2001;736–743.


16. Xie Y., Nishi S., Ueno M., Imai N., Sakatsume M., Narita I., Suzuki Y., Akazawa K., Shimada H., Arakawa M., Gejyo F.. The efficacy of tonsillectomy on long-term renal survival in patients with IgA nephropathy.
Kidney Int 63:2003;1861–1867.


17. Matsuzaki K., Suzuki Y., Nakata J., Sakamoto N., Horikoshi S., Kawamura T., Matsuo S., Tomino Y.. Nationwide survey on current treatments for IgA nephropathy in Japan.
Clin Exp Nephrol 17:2013;827–833.



18. Suzuki Y., Tomino Y.. Potential immunopathogenic role of the mucosa-bone marrow axis in IgA nephropathy: insights from animal models.
Semin Nephrol 28:2008;66–77.


19. Nakata J., Suzuki Y., Suzuki H., Sato D., Kano T., Yanagawa H., Matsuzaki K., Horikoshi S., Novak J., Tomino Y.. Changes in nephritogenic serum galactose-deficient IgA1 in IgA nephropathy following tonsillectomy and steroid therapy.
PLoS One 9:2014;e98081



20. Kawamura T., Yoshimura M., Miyazaki Y., Okamoto H., Kimura K., Hirano K., Matsushima M., Utsunomiya Y., Ogura M., Yokoo T., Okonogi H., Ishii T., Hamaguchi A., Ueda H., Furusu A., Horikoshi S., Suzuki Y., Shibata T., Yasuda T., Shirai S., Imasawa T., Kanozawa K., Wada A., Yamaji I., Miura N., Imai H., Kasai K., Soma J., Fujimoto S., Matsuo S., Tomino Y.; The Special IgA Nephropathy Study Group. A multicenter randomized controlled trial of tonsillectomy combined with steroid pulse therapy in patients with immunoglobulin A nephropathy.
Nephrol Dial Transplant 29:2014;1548–1553.






 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print
















