Outcomes of vascular access in hemodialysis patients: Analysis based on the Korean National Health Insurance Database from 2008 to 2016
Article information
Abstract
Background
Controversies exist whether arteriovenous fistula (AVF) placement is preferred over arteriovenous graft (AVG) for elderly patients. Current guidelines did not offer specific recommendations. Thus, this study was conducted to analyze the all-cause mortality and primary patency associated with various vascular access (VA) types according to age group.
Methods
This retrospective observational study investigated the Korean insurance claims data of chronic kidney disease patients who began hemodialysis between January 2008 and December 2016. We investigated all-cause mortality associated with initial VA in incident hemodialysis patients and primary patency between AVF and AVG according to age group.
Results
The proportion of patients with a tunneled dialysis catheter (TDC) that was first placed for VA increased from 18.4% in 2008 to 52.3% in 2016. Incident hemodialysis patients with a TDC or AVG for the initial VA had significantly higher mortality risk than patients with an AVF, except for patients over 85 years, who showed no significant difference in all-cause mortality regardless of VA type. In the patency analysis on initial AV access, AVG had significantly poorer primary patency than AVF in all age groups.
Conclusion
AVF had better patency than AVG in all age groups; however, the benefit of AVF attenuated in the older age groups. The mortality rate between AVF and AVG was not significantly different in patients over 85 years. Therefore, a “patient-first” approach should be emphasized over a “fistula-first” approach in AV access creation for incident hemodialysis patients older than 85 years.
Introduction
Current vascular access (VA) guidelines recommend placement of an arteriovenous fistula (AVF) over an arteriovenous graft (AVG) without specific recommendations according to patient age [1]. AVFs have superior long-term patency and fewer complications than AVGs, and some previous reports found that VA type not only contributes to patency rate, but also has an independent effect on mortality [2]. However, recent studies raised concern about whether the first choice of VA should be AVF in elderly hemodialysis (HD) patients owing to their short life expectancy and the slow maturation rate of AVF [3]. This has recently become an important issue because chronic kidney disease is a “disease of the elderly,” and the population of elderly incident HD patients has increased worldwide. The 2014 Annual Data Report of the United States Renal Data System (USRDS) reported that the mean age at the start of renal replacement therapy was 62 to 63 years, with the highest incident rates of treated end-stage renal disease (ESRD) currently in the 70- to 79-year-old age group [4].
Korea in particular has a rapidly increasing population of elderly incident HD patients [5]; therefore, to investigate the outcomes of VA, the study-population age groups should comprise patients older than 65 years. In Korea, more than 90% of ESRD patients have chosen HD as their initial renal replacement therapy modality in recent years [6]; additionally, all HD patients in Korea are undergoing HD treatment in the same, single-payer national insurance system. Hence, Korean ESRD patients are an appropriate model population to investigate the outcomes of VA in elderly patients [7]. Motivated by the above evidence, this study was conducted to analyze all-cause mortality and primary patency associated with VA type according to age group.
Methods
This retrospective, observational study was approved by the Institutional Review Board (IRB) of Hallym University Sacred Heart Hospital (IRB number: HUSHHIRB 2017-I079). Written informed consent was waived for this retrospective study.
We extracted the records of ESRD patients who underwent HD between January 2008 and December 2016 from the National Health Insurance claims database of the Health Insurance Review and Assessment Service (HIRA). The diagnosis codes were standardized according to the Korean Classification of Disease, 6th version, which follows the International Classification of Disease, 10th edition [8]. We defined ESRD patients who underwent HD as those with a diagnosis of chronic kidney disease (diagnosis code: N18 or N19), who underwent HD treatment (procedure code: O7020 or O9991), or who were given the specific code for maintenance HD patients (V001). Among these patients, we identified incident HD patients older than 18 years who had a tunneled dialysis catheter (TDC; procedure code: O7011, O7012, O7013, O7014), AVF (procedure code: O2011, O2012, O2081), or AVG (procedure code: O2082) placed as their initial VA. For these patients, we investigated all-cause mortality according to initial VA type. We also compared the primary patency between AVFs and AVGs that were created for initial permanent arteriovenous (AV) access (Fig. 1 and Supplementary Table 1, available online). Patients who had an AVF or AVG after starting HD with a TDC were classified into the AVF or AVG group, respectively, for patency analysis of initial permanent AV access.

Diagram of population selection.
AVF, arteriovenous fistula; AVG, arteriovenous graft; ESRD, end-stage renal disease; HD, hemodialysis; N, number; SD, standard deviation; TDC, tunneled dialysis catheter; VA, vascular access.
The age groups were classified as follows: young age group (18–64 years), young-old group (65–74 years), middle-old group (75–84 years), and oldest-old group (over 85 years). In the patient survival analysis, patient death was defined as discontinuation and absence of any claims data for medical service use over 30 days. In the permanent AV access patency analysis, the primary endpoint was percutaneous transluminal angioplasty (PTA; procedure code: M6597), percutaneous thrombectomy (procedure code: M6632, M6633, M6639), surgical thrombectomy or revision (procedure code: O2083), or percutaneous stent deployment (procedure code: M6605, M6613). We excluded claims data that were not related to procedures for VA of HD, such as angioplasty for renal arteries or stent placement for iliofemoral arteries. We also eliminated duplicated procedural activities, e.g., when a PTA was performed during percutaneous thrombectomy, it was regarded as a percutaneous thrombectomy case.
We presented categorical variables as frequency and percentage and continuous variables as mean and standard deviation (SD). Frequencies of VA types and age groups were compared by Pearson chi-square test for categorical variables and Student’s t test or ANOVA for continuous variables. Patient survival and access patency were assessed by Kaplan–Meier curve analysis, and the groups were compared by log-rank test or Mantel–Haenszel test. The Cox proportional-hazards model was used to estimate hazard ratios (HRs) from patient survival analysis and permanent AV access patency. We considered a finding to be statistically significant if the two-sided P value < 0.05. All analyses were conducted using R (version 3.4.1; The R Foundation for Statistical Computing, Vienna, Austria).
Results
We identified 176,331 patients with chronic kidney disease who underwent HD treatment between January 2008 and December 2016. The mean age was 58.5 years (SD, 14.6 years; median, 60 years; Q1–Q3, 49–70 years; range, 1–115 years). Among them, we identified 87,536 incident HD patients older than 18 years who underwent TDC, AVF, or AVG placement as their initial VA (Table 1). The mean age in these incident HD patients was 62.2 years (SD, 14.1 years; median, 64 years; Q1–Q3, 53–73 years; range, 18–105 years). The numbers and proportions of patients in the young age group, young-old group, middle-old group, and oldest-old group were 45,634 (52.1%), 23,230 (26.5%), 15,882 (18.1%), and 2,790 (3.2%), respectively (Supplementary Table 2).
The number of incident HD patients initiating maintenance HD with a TDC increased rapidly over the study period, while the number of those who had an AVF as their initial VA decreased (Fig. 2). The proportion of ESRD patients with a TDC as their initial VA, which was 18.4% in 2008, continued to increase, reaching 52.3% in 2016, while that of the patients who had an AVF as their first-placed VA decreased from 64.9% to 38.3% during the same period.
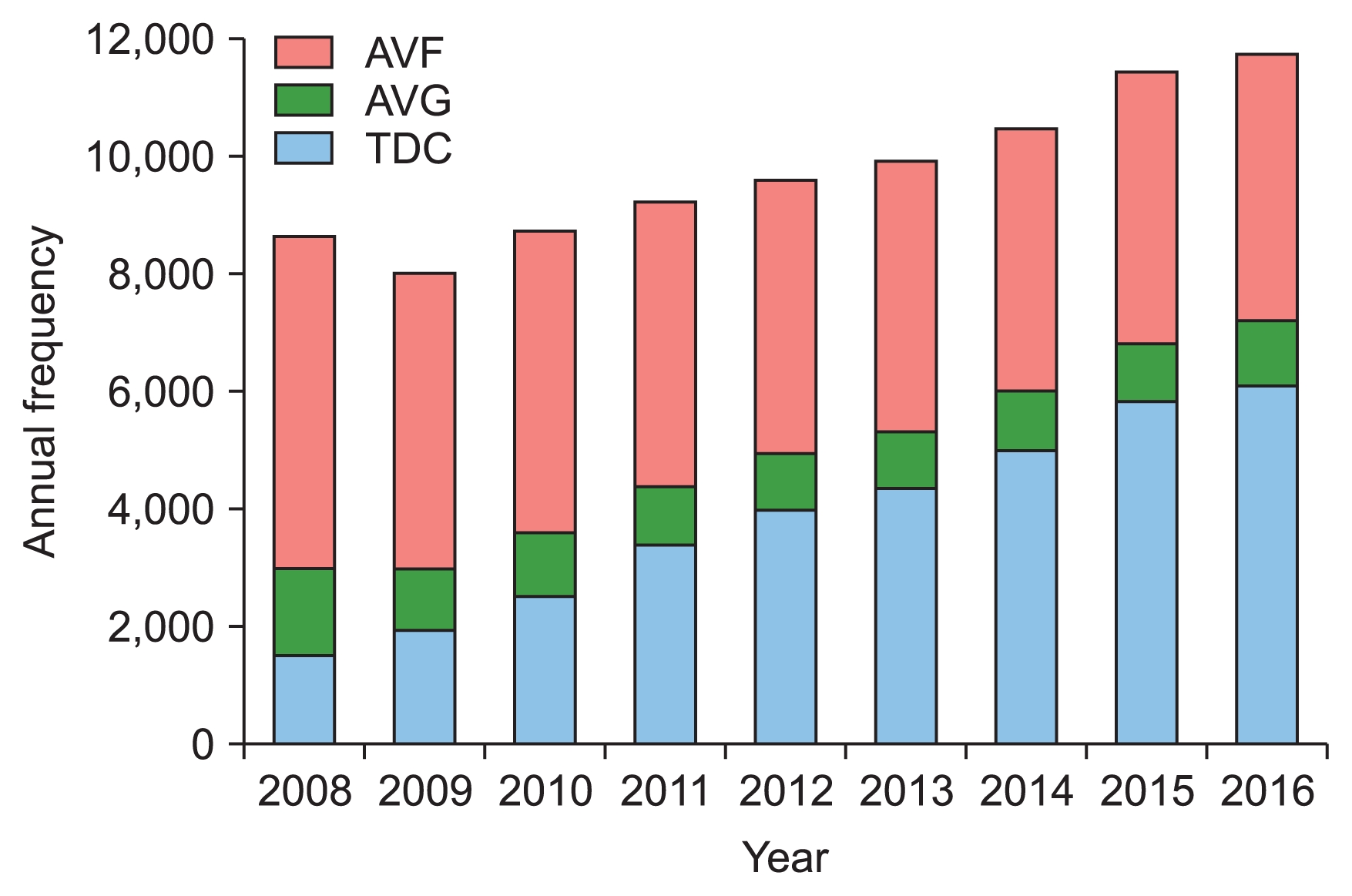
Annual frequency and proportion of initial vascular access.
AVF, arteriovenous fistula; AVG, arteriovenous graft; TDC, tunneled dialysis catheter.
The overall survival of incident HD patients who had an AVF as their initial VA was significantly better than that of those who had a TDC or AVG according to Mantel–Haenszel tests for survival (P < 0.001) and the Kaplan–Meier survival curve (Fig. 3A). In Cox proportional hazards analysis after stratification for sex and age groups, the HR of all-cause mortality for the AVG and TDC groups against the AVF group presented as 1.40 (P < 0.001; 95% CI, 1.35–1.45) and 1.93 (P < 0.001; 95% CI, 1.89–1.98), respectively. This suggests that patients with a TDC or AVG as their initial VA had poorer survival than those with an AVF. However, the survival benefit of AVFs compared with AVGs was not statistically different in the oldest-old group (over 85 years) according to the Kaplan–Meier survival curve (Fig. 3B) and Cox proportional hazards analysis after stratification for sex (HR, 1.12; P = 0.196; 95% CI, 0.94–1.34; Table 2).
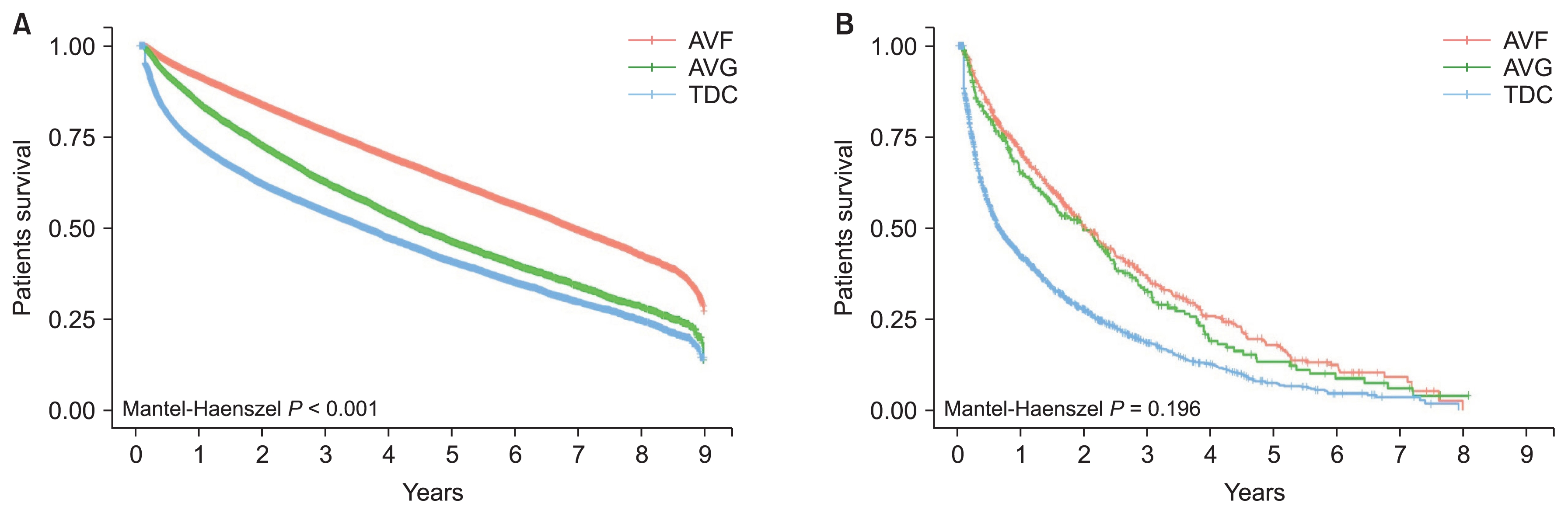
Patient survival according to the type of initial vascular access.
(A) Overall patient survival according to the type of initial vascular access. (B) Patient survival according to the type of initial vascular access in the oldest-old group (over 85 years old).
AVF, arteriovenous fistula; AVG, arteriovenous graft; TDC, tunneled dialysis catheter.
To compare the primary patency of initial permanent AV access between AVFs and AVGs according to age group, we identified 73,939 adult incident HD patients who had an AVF or AVG as their initial permanent AV access. Mean patient age was 61.5 years (SD, 13.6 years; median, 63 years; Q1–Q3, 52–72 years; range, 18–105 years). The numbers and proportions of patients in the AVF and AVG groups were 59,753 (80.8%) and 14,186 (19.2%), respectively (Table 3). Although the proportion of AVG as an initial permanent AV access was higher in the older groups, more than 66% of the incident HD patients over 85 years who underwent permanent AV access had an AVF as their initial permanent AV access. Primary AV access placement has increased along with the incident HD patient population from 2008 to 2016, and AVF as the initial permanent AV access has been steadily increasing to four times greater than AVG (Fig. 4 and Supplementary Table 3). The incident HD patients who had an AVG as their initial permanent AV access underwent more frequent salvage procedures such as PTA, stent placement, percutaneous thrombectomy, and surgical revision (Table 4). The overall primary patency of AVF as the initial permanent AV access was significantly better than that of AVG according to the log-rank test for survival analysis (P < 0.001) and Kaplan–Meier survival curves (Fig. 5A). In Cox proportional hazards analysis after stratifying for sex, age group, and TDC history, patients with an AVG as their initial permanent AV access had poorer primary patency than patients with an AVF, with an estimated HR of 1.7 (P < 0.001; 95% CI, 1.68–1.75; Table 5). A relative benefit of AVF patency was present among all age groups in the Cox proportional hazards analysis after stratification, but it was attenuated in the oldest-old group (Fig. 5B).
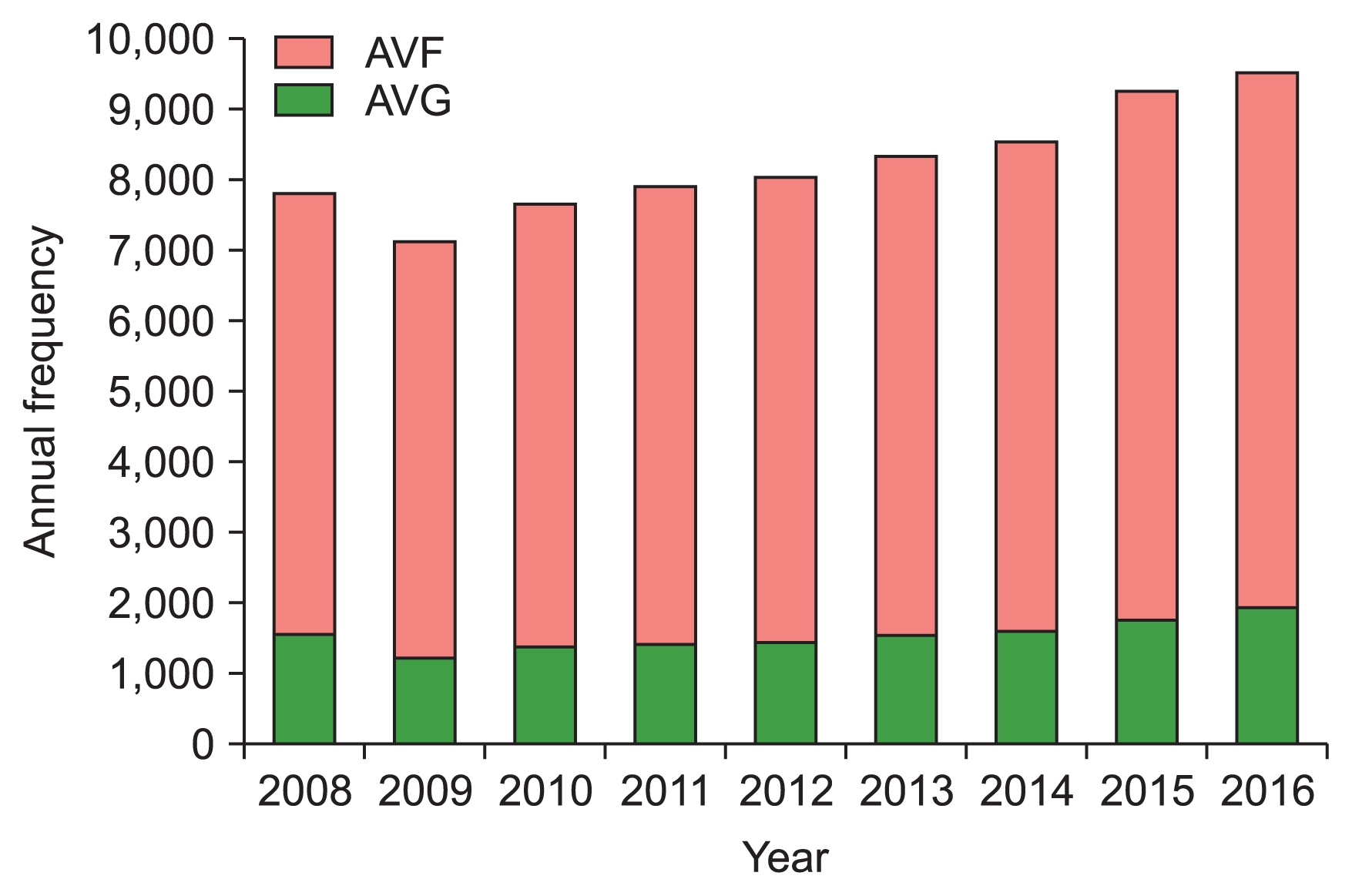
Annual frequency and proportion of initial permanent arteriovenous access.
AVF, arteriovenous fistula; AVG, arteriovenous graft.
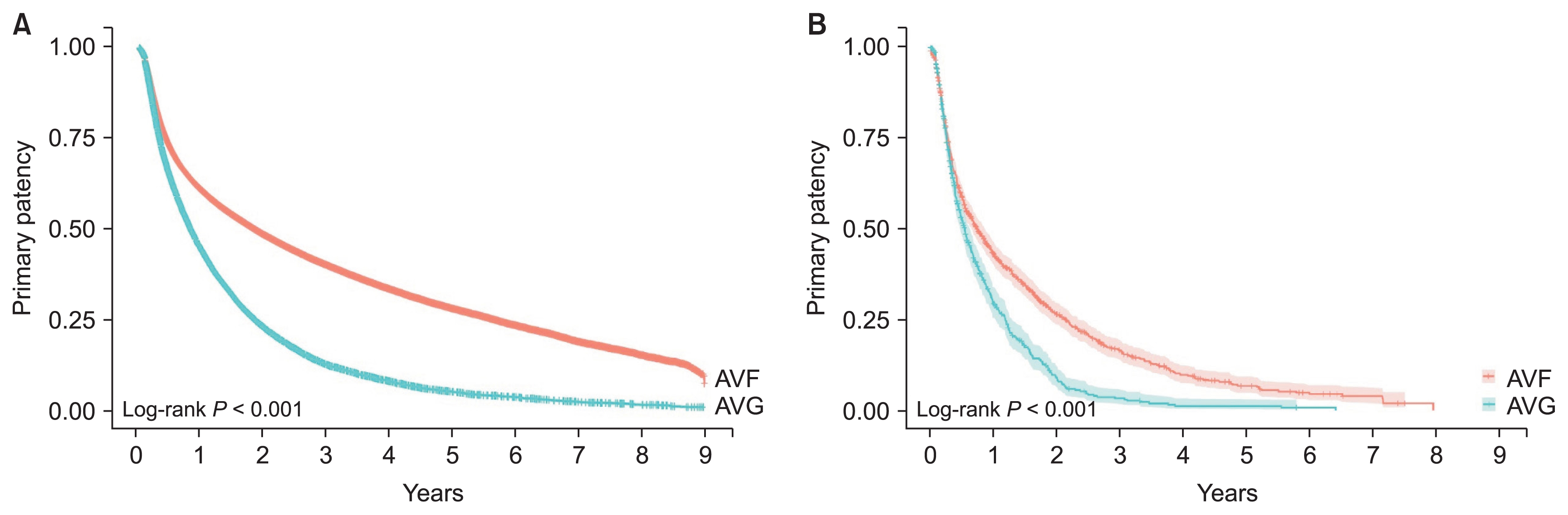
Primary patency according to the type of initial permanent arteriovenous access.
(A) Overall primary patency according to the type of initial permanent arteriovenous access. (B) Primary patency according to the type of initial permanent arteriovenous access in the oldest-old group (over 85 years old).
AVF, arteriovenous fistula; AVG, arteriovenous graft.
Discussion
As age increases, it becomes more challenging to place an ideal VA in elderly ESRD patients, and there are controversies about whether the “fistula-first” approach should be uniformly applied to elderly patients. Korea has one of the fastest growing populations of elderly HD patients in the world, and more than 90% of patients start renal replacement therapy with HD [6]. Therefore, whether the “fistula-first” approach should be also applied in elderly patients is a crucial issue in Korea; however, no large population-based studies have investigated VA outcomes according to age or current status of VA in Korea.
In this study, we found that the proportion of patients who had a TDC as their initial VA increased rapidly over time, reaching 52.2% in 2016. The incident HD patients in the older age group had a larger proportion of TDCs as their first-placed VA. Therefore, the growing number of elderly ESRD patients might have contributed to the increase in TDC placement. Although it is a small proportion compared to USRDS data, which reported a TDC proportion of about 80% [9], the rapidly increasing TDC trend is noteworthy. Central venous catheter (CVC) has been reported to be associated with increased mortality compared with AVF or AVG because of its associated complications, including infection [10]. However, Ravani et al [11] noted that the mortality rate owing to the catheter itself was only 2%, and incident HD patients with catheter experienced higher mortality rates because they were more likely to have comorbidities.
Currently, no randomized controlled trial has been conducted on the associations between VA type and outcomes; hence, most previous reports based on observational studies could not exclude potential selection biases. This problem also arose in previous analyses of mortality rates between AVFs and AVGs. HD patients with an AVF as their initial VA are likely to be less morbid than patients with an AVG; thus, lower morbidity may be a confounding factor of the better survival rate among the AVF group. Considering that bias likely favors AVFs, the results of this study, which found no statistical difference in all-cause mortality between AVF and AVG in the oldest-old group, raise strong doubt about the application of the “fistula-first” policy for incident HD patients older than 85 years. Our results are consistent with recent reports that AVF had no survival benefit over AVG in HD patients older than 80 years [12].
AVFs have fewer complications once they mature, but they take more time to mature and are associated with a competing risk of death until the patient begins to derive benefits. Therefore, patient life expectancy becomes an important concern [13]. Viecelli and Lok [14] reported that high morbidity in elderly patients and the risk of a short lifespan offset the benefit of AVF over AVG. In the present study, the survival benefit of AVF decreased as patient age increased; therefore, in elderly ESRD patients, individualized VA selection that considers patient morbidity, short life expectancy, and personal preference is necessary, especially for patients older than 85 years.
In the patency analysis of permanent AV access, a comparison of the frequency and proportion of AVFs and AVGs showed that the rate of AVF placement as the initial permanent AV access was consistently much higher than for AVG, even in elderly HD patients. From 2008 to 2016 in Korea, 66.4% of the elderly incident HD patients older than 85 years underwent AVF for initial permanent AV access. AVF placement in elderly patients has been reported to require more maturation-enhancing procedures to achieve maturation [15], which reflects a tradeoff between maturation and maintenance procedures [16]. We compared the frequency of salvage procedures, including PTA, stent placement, percutaneous thrombectomy, and surgical revision, between the AVF and AVG groups and found that more salvage procedures were required in the AVG group. This implies that the need for AVG maintenance procedures is greater than the need for AVF maturation procedures. Therefore, although AVFs require a longer maturation and maturation-enhancing procedures, AVF creation is more advantageous than AVG placement given the necessity for salvage procedures.
Our comparative analysis of primary patency between AVFs and AVGs found that AVFs showed significantly better primary patency in all age groups; even in the oldest-old group (> 85 years), AVF was more beneficial if the vascular state was adequate. Although good candidate vessels for AVF placement are less frequently encountered in older patients, AVF creation is recommended regardless of age if a high possibility of maturation is anticipated based on the likelihood estimated by the maturation algorithm, as presented in a previous report [17].
This study has all the limitations inherent to an observational study. For more robust conclusions, more detailed investigations, including propensity-score matching, are needed to account for the relatively small number and short life span of patients older than 85. Additionally, we did not include non-tunneled temporary catheter cases, and our design was a Korean population-based study; thus, the results could not be generalized to the HD population at large. Furthermore, we were not able to analyze comorbidities such as diabetes mellitus, cardiovascular disease, peripheral arterial disease, and dyslipidemia, because the HIRA database did not include results from diagnostic examinations, and the diagnostic codes from claims data were not sufficiently accurate. A reliable method to reasonably screen comorbid disease from the HIRA database should be developed and applied to future studies.
In conclusion, AVF offered superior primary patency to AVG, but the benefit attenuated with increasing age. Therefore, clinical practitioners need to consider life expectancy, vessel status, and patient preference before planning AV access. Moreover, because patient survival was not significantly different between the AVF and AVG groups among incident HD patients older than 85 years, it is necessary to reassess whether the “fistula-first” policy should be similarly applied across all age groups.
Supplementary Information
Notes
Contributed by the Korean Society of Diagnostic and Interventional Nephrology
Conflicts of interest
All authors have no conflicts of interest to declare.
Authors’ contributions
Hyung Seok Lee, Young Rim Song participated in the data collection and wrote the manuscript. Jwa Kyung Kim, Narae Joo, and Cheolsu Kim participated in the study design and performed the statistical analysis. Sung Gyun Kim participated in the conception, analysis, and interpretation of data. Hyung Seok Lee, and Sung Gyun Kim provided intellectual content of critical importance to the work and technical support. Hyung Jik Kim participated in the study design and coordination and helped to draft the manuscript. All authors read and approved the final manuscript.




