1. Cooper C, Campion G, Melton LJ 3rd. Hip fractures in the elderly: a world-wide projection.
Osteoporos Int 1992;2:285ŌĆō289.


2. Hailer NP, Garland A, Rogmark C, Garellick G, K├żrrholm J. Early mortality and morbidity after total hip arthroplasty in patients with femoral neck fracture.
Acta Orthop 2016;87:560ŌĆō566.



3. Griffin XL, Parsons N, Achten J, Fernandez M, Costa ML. Recovery of health-related quality of life in a United Kingdom hip fracture population. The Warwick Hip Trauma Evaluation: a prospective cohort study.
Bone Joint J 2015;97-B:372ŌĆō382.

4. Hobson C, Ozrazgat-Baslanti T, Kuxhausen A, et al. Cost and mortality associated with postoperative acute kidney injury.
Ann Surg 2015;261:1207ŌĆō1214.



5. Coca SG, Yusuf B, Shlipak MG, Garg AX, Parikh CR. Long-term risk of mortality and other adverse outcomes after acute kidney injury: a systematic review and meta-analysis.
Am J Kidney Dis 2009;53:961ŌĆō973.



6. Lafrance JP, Miller DR. Acute kidney injury associates with increased long-term mortality.
J Am Soc Nephrol 2010;21:345ŌĆō352.



7. Anderson S, Eldadah B, Halter JB, et al. Acute kidney injury in older adults.
J Am Soc Nephrol 2011;22:28ŌĆō38.


8. Denic A, Glassock RJ, Rule AD. Structural and functional changes with the aging kidney.
Adv Chronic Kidney Dis 2016;23:19ŌĆō28.



9. Villari B, Vassalli G, Schneider J, Chiariello M, Hess OM. Age dependency of left ventricular diastolic function in pressure overload hypertrophy.
J Am Coll Cardiol 1997;29:181ŌĆō186.


10. Burlew BS. Diastolic dysfunction in the elderly--the interstitial issue.
Am J Geriatr Cardiol 2004;13:29ŌĆō38.

11. Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group.
Ann Intern Med 1999;130:461ŌĆō470.


12. Thomas ME, Blaine C, Dawnay A, et al. The definition of acute kidney injury and its use in practice.
Kidney Int 2015;87:62ŌĆō73.


13. Siew ED, Ikizler TA, Matheny ME, et al. Estimating baseline kidney function in hospitalized patients with impaired kidney function.
Clin J Am Soc Nephrol 2012;7:712ŌĆō719.



14. Siew ED, Matheny ME. Choice of reference serum creatinine in defining acute kidney injury.
Nephron 2015;131:107ŌĆō112.



15. Biteker M, Dayan A, Tekke┼¤in A─░, et al. Incidence, risk factors, and outcomes of perioperative acute kidney injury in noncardiac and nonvascular surgery.
Am J Surg 2014;207:53ŌĆō59.


16. Kheterpal S, Tremper KK, Heung M, et al. Development and validation of an acute kidney injury risk index for patients undergoing general surgery: results from a national data set.
Anesthesiology 2009;110:505ŌĆō515.


17. Cho EJ, Cha IH, Yoon KC, et al. Clinical characteristics and outcomes of septic acute kidney injury in critically ill patients. Kidney Res Clin Pract 2011;30:253ŌĆō259.
18. Shiao CC, Wu PC, Huang TM, et al. National Taiwan University Hospital Study Group on Acute Renal Failure (NSARF) and the Taiwan Consortium for Acute Kidney Injury and Renal Diseases (CAKs). Long-term remote organ consequences following acute kidney injury.
Crit Care 2015;19:438



19. Thakar CV. Perioperative acute kidney injury.
Adv Chronic Kidney Dis 2013;20:67ŌĆō75.


20. Sun LY, Wijeysundera DN, Tait GA, Beattie WS. Association of intraoperative hypotension with acute kidney injury after elective noncardiac surgery.
Anesthesiology 2015;123:515ŌĆō523.


21. Lim SY, Lee JY, Yang JH, et al. Predictive factors of acute kidney injury in patients undergoing rectal surgery.
Kidney Res Clin Pract 2016;35:160ŌĆō164.



22. Goren O, Matot I. Perioperative acute kidney injury.
Br J Anaesth 2015;115(Suppl 2):ii3ŌĆōii14.


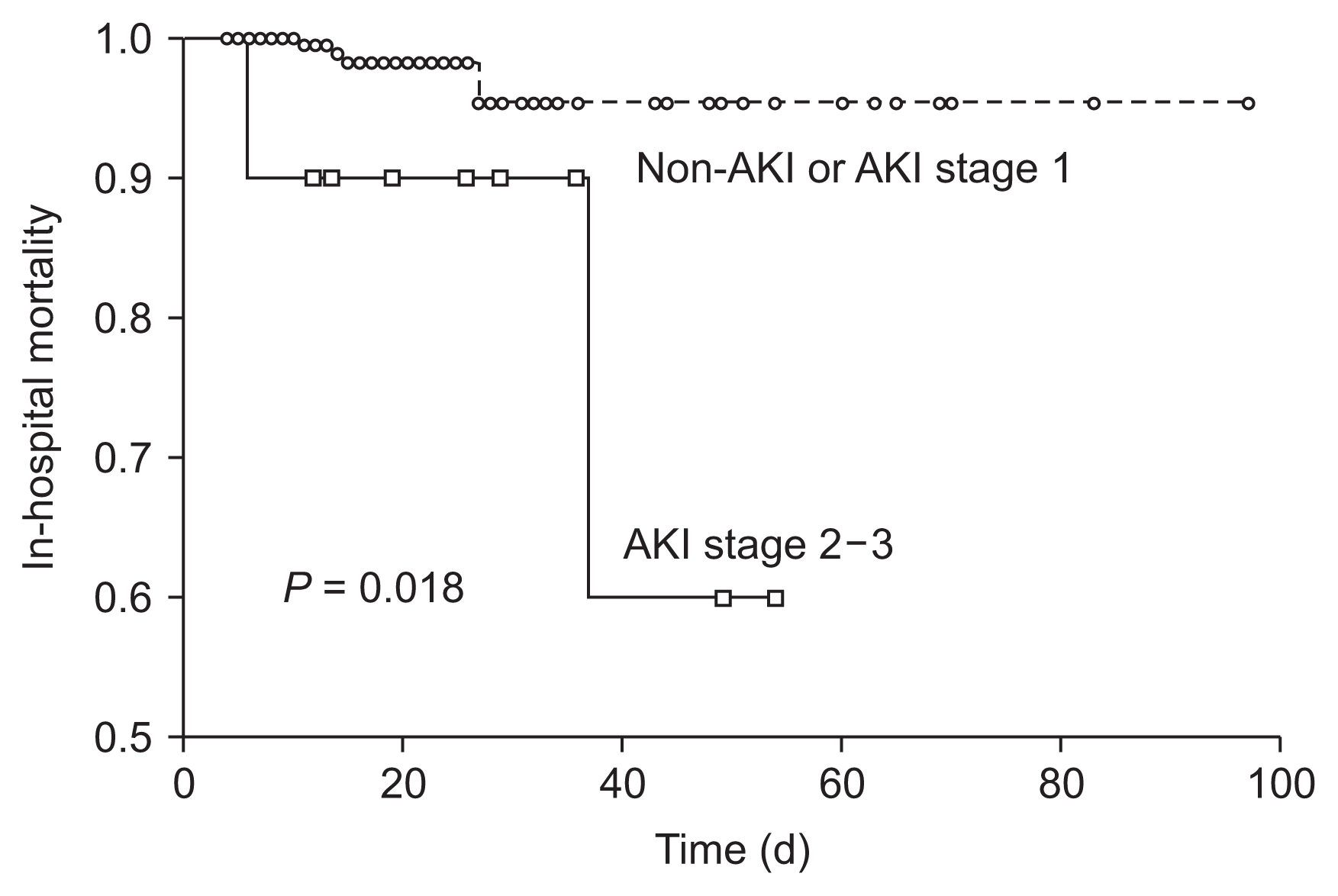
23. Hong SE, Kim TY, Yoo JH, et al. Acute kidney injury can predict in-hospital and long-term mortality in elderly patients undergoing hip fracture surgery.
PLoS One 2017;12:e0176259



24. Ulucay C, Eren Z, Kaspar EC, et al. Risk factors for acute kidney injury after hip fracture surgery in the elderly individuals.
Geriatr Orthop Surg Rehabil 2012;3:150ŌĆō156.



25. Golden D, Corbett J, Forni LG. Peri-operative renal dysfunction: prevention and management.
Anaesthesia 2016;71(Suppl 1):51ŌĆō57.


26. McKinlay J, Tyson E, Forni LG. Renal complications of anaesthesia.
Anaesthesia 2018;73(Suppl 1):85ŌĆō94.


27. Abelha FJ, Botelho M, Fernandes V, Barros H. Determinants of postoperative acute kidney injury.
Crit Care 2009;13:R79



28. Redfield MM. Heart failure with preserved ejection fraction.
N Engl J Med 2016;375:1868ŌĆō1877.


29. Nagueh SF, Appleton CP, Gillebert TC, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography.
J Am Soc Echocardiogr 2009;22:107ŌĆō133.


30. OŌĆÖRouke RA, Hurst JW. HurstŌĆÖs the heart: Manual of cardiology. 10th ed. New York: McGraw-Hill; 2001. p. 658ŌĆō660.
31. Anand IS. Cardiorenal syndrome: a cardiologistŌĆÖs perspective of pathophysiology.
Clin J Am Soc Nephrol 2013;8:1800ŌĆō1807.



32. Han SS, Park S, Kang SH, et al. Usefulness of preoperative echocardiography to predict acute kidney injury and long-term mortality after coronary artery bypass grafting.
Am J Cardiol 2017;119:231ŌĆō236.


33. Hur M, Nam K, Jo WY, Kim G, Kim WH, Bahk JH. Association between elevated echocardiographic index of left ventricular filling pressure and acute kidney injury after off-pump coronary artery surgery.
Circ J 2018;82:857ŌĆō865.


34. Flint N, Kaufman N, Gal-Oz A, et al. Echocardiographic correlates of left ventricular filling pressures and acute cardio-renal syndrome in ST segment elevation myocardial infarction patients.
Clin Res Cardiol 2017;106:120ŌĆō126.


35. Muhm M, Amann M, Hofmann A, Ruffing T. Changes in the patient population with proximal femur fractures over the last decade : incidence, age, comorbidities, and length of stay. Unfallchirurg 2018 121:649ŌĆō656. German.
36. Neuman Y, Kotliroff A, Bental T, Siegel RJ, David D, Lishner M. Pulmonary artery pressure and diastolic dysfunction in normal left ventricular systolic function.
Int J Cardiol 2008;127:174ŌĆō178.


37. Teo SG, Yang H, Chai P, Yeo TC. Impact of left ventricular diastolic dysfunction on left atrial volume and function: a volumetric analysis.
Eur J Echocardiogr 2010;11:38ŌĆō43.


38. Kimura H, Takeda K, Tsuruya K, et al. Left ventricular mass index is an independent determinant of diastolic dysfunction in patients on chronic hemodialysis: a tissue Doppler imaging study.
Nephron Clin Pract 2011;117:c67ŌĆōc73.


39. Kim JS, Yang JW, Yoo JS, Choi SO, Han BG. Association between E/├® ratio and fluid overload in patients with predialysis chronic kidney disease.
PLoS One 2017;12:e0184764






 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print
















