Weight loss has an additive effect on the proteinuria reduction of angiotensin II receptor blockers in hypertensive patients with chronic kidney disease
Article information
Abstract
Background
Weight reduction is a lifestyle intervention that has been introduced for prevention and management of chronic kidney disease (CKD). We investigate the additive anti-proteinuric effect of weight reduction on the usage of angiotensin II receptor blockers (ARBs) and its potential mechanisms in hypertensive CKD patients.
Methods
This study is a subanalysis of data from an open-label, randomized, controlled clinical trial. Among the 235 participants, 227 were assigned to subgroups according to changes in body weight.
Results
Fifty-eight participants (25.6%) were assigned to group 1 (≥1.5% decrease in body weight after 16 weeks), 32 participants (14.1%) were assigned to group 2 (1.5–0.1% decrease in body weight), and 136 participants (59.9%) were assigned to group 3 (≥ 0.0% increase in body weight). Characteristics at enrollment were not different among the three groups, but mean differences in weight and percent changes in urinary sodium excretion over the period were statistically different (P < 0.001 and P = 0.017). Over the study period, unintentional weight loss independently increased the probability of reduced albuminuria (group 1, relative risk 6.234, 95% confidence interval 1.913–20.315, P = 0.002). Among urinary cytokines, only podocalyxin level decreased significantly in participants who lost weight (P = 0.013).
Conclusion
We observed that weight loss had an additive effect on the anti-proteinuric effects of ARBs in nondiabetic hypertensive CKD patients, although it was minimal. An additive effect was shown in both obese and non-obese participants, and its possible mechanism is related to reduction of podocyte damage.
Introduction
Chronic kidney disease (CKD) is a well-known risk factor for end-stage renal disease (ESRD), hospitalization, cardiovascular morbidity and mortality, and general mortality [1,2]. Because the incidence and prevalence of diabetes and hypertension, leading causes of CKD, have increased consistently [3,4], CKD is a common disease worldwide [5,6]. However, in recent years, the prevalence of CKD has plateaued in the United States [6] and decreased in the United Kingdom [7], which may be due to improved strategies for CKD management.
Several strategies have been established for clinical care of CKD patients, including blood pressure (BP) control, reduced proteinuria through the use of renin-angiotensin system (RAS) blockers, correction of hyperglycemia and dyslipidemia, avoidance of nephrotoxic drugs, and lifestyle modifications such as low salt diet and protein restriction [8,9]. Weight reduction through restricted diets, exercise therapy, anti-obesity drugs, and bariatric surgery is another commonly used lifestyle intervention. Traditionally, weight gain and obesity have contributed to the development of CKD and ESRD [10,11]. For that reason, weight reduction has been considered important for management of CKD [5,12]. However, the evidence in support of these concepts was based on studies that involved obese CKD patients. The majority of these studies excluded participants with body mass index (BMI) < 25 kg/m2. Therefore, the clinical implications of weight loss in patients with CKD should be explored, even if patients are not obese or the degree of weight loss is minimal.
This is a subanalysis result of an open-label, case-controlled, randomized clinical trial exploring the proteinuria-lowering effects of a low salt diet in nondiabetic, hypertensive CKD patients taking RAS blockers [13]. All participants in the study were prescribed RAS blockers to control BP and reduce proteinuria and were educated about low-salt diet (LSD), although the intensity of education differed. Even if not intended, the weight of participants changed during the study period. The additive effects of unintentional weight loss on clinical progression of study participants taking RAS blockers and the potential mechanisms of those effects were evaluated.
Methods
Study population
This study involved a subsequent analysis of data from an open-label, case-controlled, randomized clinical trial (NCT01552954) [13]. The patients were selected from outpatient renal clinics of 7 centers in Korea between March 2012 and March 2013. All participants fulfilled the following inclusion criteria: between 19 and 75 years of age; use of antihypertensive medication or a diagnosis of hypertension; Modification of Diet in Renal Disease (MDRD)-estimated glomerular filtration rate (eGFR) ≥ 30 mL/min/1.73 m2; random urine albumin to creatinine ratio ≥ 30 mg/g Cr in the last 6 months; and the ability and willingness to provide written informed consent. The exclusion criteria were as follows: uncontrolled hypertension (BP > 160/100 mmHg) at the time of screening; pregnancy; serum potassium > 5.5 mEq/L; malignancy; diagnosis of cardiovascular disease (cerebral infarction, hemorrhagic infarction, acute myocardial infarction or unstable angina, coronary angioplasty, or coronary artery bypass surgery) within the last 6 months; contraindication to angiotensin II receptor blockers (ARBs); diabetes mellitus; and the use of steroids or other immunosuppressive agents at the time of registration.
The sample size was calculated according to a reference from a specific article with proteinuria as an outcome [14]. A two-sided 5% significance level, power of 80%, and sample size of 135 patients per group were necessary given an anticipated dropout rate of 20%. To recruit this number of patients, a 12-month inclusion period was anticipated. During the study period, 312 patients were screened, 269 patients were enrolled, 34 patients dropped out, and 235 patients completed the trial (Fig. 1). Among 235 participants, 227 provided body weight and 24-hour urine samples at baseline and after 16 weeks.
Study protocol
The patients were screened 8 weeks prior to commencement of the study. The protocol included a “run-in period” for adjustment of antihypertensive medications. All participants were instructed to stop any RAS blocking agents or diuretic therapies and to switch to antihypertensive agents of different categories during this period. After an 8-week run-in period (0-week), the investigators conducted baseline laboratory investigations. From the 0-week time point, all enrolled patients were prescribed olmesartan medoxomil (Daewoong Pharmaceutical Co./Daiichi Sankyo Korea Co., Seoul, Korea) at a 40 mg daily fixed dose until the end of the study. After another 8 weeks (week 8), participants were randomly assigned (1:1) to either conventional education (control) or intensive education for LSD using computerized block randomization with block size six and balanced according to institution and gender. It was not feasible to mask participants to allocation, but clinicians were masked to group assignment. Participants in the conventional education group received routine LSD education at an outpatient clinic. Participants in the intensive education group were closely supported by a dietary consultant and provided feedback by telephone for 30 minutes once a week during the study period.
After 16 weeks (16-week), participants again underwent a laboratory investigation. At the 0- and 16-week time points, patients were asked to collect 24-hour urine samples on the day before each visit to assess albuminuria, urinary sodium, urea nitrogen, and creatinine excretion (Supplementary Fig. 1; available at https://doi.org/10.23876/j.krcp.2018.37.1.49). Some urine samples from the 24-hour urine collection were stored in a refrigerator at −70°C for future measurements of urine cytokine levels. Compliance was assessed using the 24-hour urine samples with correction by calculating the predicted daily creatinine excretion (male: −12.63 × age + 15.12 × body weight + 7.39 × height − 79.9 mg/day; female: −4.72 × age + 8.58 × body weight + 5.09 × height − 74.5 mg/day) [15]. Participants with poor medication adherence to olmesartan (used ≤ 60% of the prescribed medication) were removed from the study. During the 16 weeks, no medications were changed, other than olmesartan medoxomil, to adjust and maintain BP at 130/80 mmHg, and none of the participants were prescribed diuretics. BP measurements were performed when patients visited the clinic. The sphygmomanometer differed depending on the institution, and the number of measurements was not confirmed. Safety assessments included adverse events, self-reported hypotension, and select hematological and biochemical measures.
Ethics approval and consent to participate
The protocol was approved by the Institutional Review Board (IRB) of Seoul National University Bundang Hospital (IRB no. B-1112-142-008). The study procedures were in accordance with the ethical standards of the IRB of Seoul National University Bundang Hospital and the 2008 Helsinki Declaration. Written informed consent was obtained from each participant prior to inclusion.
Outcome measurements
The additive anti-proteinuric effects of weight reduction on usage of an ARB were analyzed, and the potential mechanisms of those effects in hypertensive CKD patients were explored.
Weight measurement
At the 0- and 16-week time points, participant body weights were measured using a scale. Participants were assigned to the following subgroups according to changes in body weight during the 16 weeks by the ratio of body weight at week 16 compared to week 0: 1) group 1, patients with ≥ 1.5% decrease; 2) group 2, patients with 1.5% to 0.1% decrease; and 3) group 3, patients with ≥ 0.0% increase.
Cytokine measurements
Several urinary cytokines including angiotensinogen (AGT), malondialdehyde (MDA), monocyte chemoat-tractant protein-1 (MCP-1), adiponectin, and podocalyxin were measured. Urinary concentrations of AGT were measured with a Human AGT ELISA Kit (Cat No. CSB-E08564h; Cusabio Biotech, College Park, MD, USA), MDA was measured with MDA assay kits (Cat No. STA-330; Cell Biolab, Inc., San Diego, CA, USA), MCP-1 was measured with a Human MCP-1 ELISA Kit (Quantikine kit; R&D Systems, Abingdon, UK), adiponectin was measured with a highly sensitive ELISA (BioVendor, Brno, Czech), and podocalyxin was measured with human ELISA kit (Cat No. CSB-E09891h; Cusabio Biotech) according to the manufacturers’ protocols. All cytokine concentrations were measured in duplicate and adjusted for urinary creatinine concentration.
Statistical analysis
The urine marker-to-creatinine ratio (a unit/g creatinine) was multiplied by calculating the estimated creatinine excretion rate (eCER) (g/24 hour) to obtain the estimated urine excretion of a marker (in a unit/24 hour)[16]. The equations suggested by Tanaka et al [17] were used to calculate eCER. Protein intake was calculated as follows: “24-hour urine urea nitrogen [17] + {body weight [18] × 0.031 (g nitrogen/kg/day)} × 6.25 (g protein/day)” and normalized to body weight (g protein/kg body weight/ day). Differences in the parameters between 16- and 0-week values were calculated, as well as the percentage change; “(value at 16-week – value at 0-week) × 100/ value at 0-week (%)”. Decreases in albuminuria and urine cytokines were defined based on the ratios of estimated albuminuria and urine cytokines at the 16-week time point compared with those at the 0-week time point and were ≤ −25%.
All analyses and calculations were performed using SPSS Statistics ver. 21.0 (IBM Co., Armonk, NY, USA). Continuous variables were expressed as the mean ± standard deviation or as a percentage for categorical variables. The Kruskal–Wallis test was used to compare continuous variables between groups, and the Pearson’s chi-square test or linear by linear chi-square statistic was used to analyze associations between categorical variables. The relationships between variables were estimated using Pearson’s correlation coefficient and tested using multiple linear regression analysis for continuous variables and multiple logistic regression analysis for dichotomized variables by adjusting for related factors. Two-tailed values of P < 0.05 were considered statistically significant.
Results
Baseline characteristics of participants
The mean age at enrollment was 50.3 ± 13.0 years, and 50% of participants were male. The mean BMI was 25.4 ± 3.8 kg/m2, and approximately 53.7% of subjects were obese (BMI ≥ 25 kg/m2) (Supplementary Table 1; available at https://doi.org/10.23876/j.krcp.2018.37.1.49). Participants were assigned to three groups according to the change in body weight after 16 weeks. Fifty-eight participants (25.6%) were assigned to group 1 (≥ 1.5% decrease in body weight after 16 weeks), 32 participants (14.1%) were assigned to group 2 (1.5–0.1% decrease in body weight after 16 weeks), and 136 participants (59.9%) were assigned to group 3 (≥ 0.0% increase in body weight after 16 weeks) (Table 1). Group 3 had the highest mean age, total cholesterol level, eGFR, and amount of estimated protein intake using the estimated level of urine urea nitrogen, as well as the lowest mean BMI at enrollment. However, the differences were not statistically significant. Other baseline characteristics at enrollment including BP, comorbidities, and medication use were also not different among the three groups.
The mean differences in weight over the period were statistically significant; −2.41 ± 1.45 kg in group 1, −0.55 ± 0.33 kg in group 2, and 1.28 ± 1.74 kg in group 3 (P < 0.001). The percent changes in other parameters during the 16 weeks were also evaluated according to group (Table 2). The ratios of estimated protein intake, systolic BP (SBP), total cholesterol, and eGFR between the 16- and 0-week time points did not significantly differ among the three groups. In other words, there was no evidence that clinical status was getting worse in the weight-loss group. However, the percent change in urinary sodium excretion, which indicates the change in salt intake over the 16 weeks, was significantly different among the three groups (P = 0.017), and the proportion of change among the intensive education group was remarkably higher for those who lost weight, as expected (P = 0.003).
Changes in body weight and decreases in albuminuria
Next, the percent change in albuminuria over the 16 weeks was compared among the three groups using the Kruskal–Wallis test (Fig. 2A). With a greater decrease in body weight over the 16 weeks, there was a greater decrease in albuminuria. The percentage of participants who achieved > 25% decrease in albuminuria after treatment with ARB compared with baseline was 93.0% in group 1, 80.6% in group 2, and 71.1% in group 3 (Fig. 2B). Multiple logistic regression analysis was also used to evaluate the independent factors for predicting > 25% decrease in albuminuria after 16 weeks adjusting for age, sex, and other factors related to decreased albuminuria level, such as albuminuria at baseline; percent changes in SBP, diastolic BP, eGFR, total CO2, serum total cholesterol, and 24-hour urine excretion of sodium; and group change in body weight (Table 3). As shown in Table 3, the probability of decreased albuminuria with ARB treatment was higher in the study population with baseline albuminuria and reduced body weight. In particular, the participants in group 1 (with ≥ 1.5% decrease in body weight after 16 weeks) showed the highest probability of decreased albuminuria level. The interactions were explored between change in body weight and other independent factors, such as baseline albuminuria, change in SBP, estimated urinary sodium excretion, and estimated protein intake over 16 weeks. There were no interactions between changes in body weight and the other independent factors.

Decreased albuminuria according to change in body weight during the 16-week study period
(A) Percent change in albuminuria over 16 weeks. (B) Percentage of participants who achieved > 25% decrease in albuminuria. Group 1 (≥ 1.5% decrease in body weight), group 2 (1.5–0.1% decrease in body weight), and group 3 (≥ 0.0% increase in body weight). The bar represents the 95% confidence interval of the mean value.
P values were estimated by *Kruskal–Wallis test and †Pearson’s chi-square test.
Changes in body weight and decreases in urinary cytokines
Finally, correlations between the frequencies of reduced cytokines and changes in weight were assessed. Participants with reduced body weight had a higher frequency of decreases in the following urinary cytokines after 16 weeks: adiponectin, AGT, MCP-1, MDA, and podocalyxin (Fig. 3). However, only the decrease in podocalyxin, a marker of podocyte injury, was statistically significant across groups (P = 0.013). Next, factors related to the decrease in podocalyxin were examined. Among baseline clinical parameters, estimated urine albumin excretion was an independent risk factor. The ratio of estimated urine albumin excretion at the 16-week time point compared to the 0-week time point also showed the probability of a decrease in podocalyxin (Supplementary Table 2; available at https://doi.org/10.23876/j.krcp.2018.37.1.49).
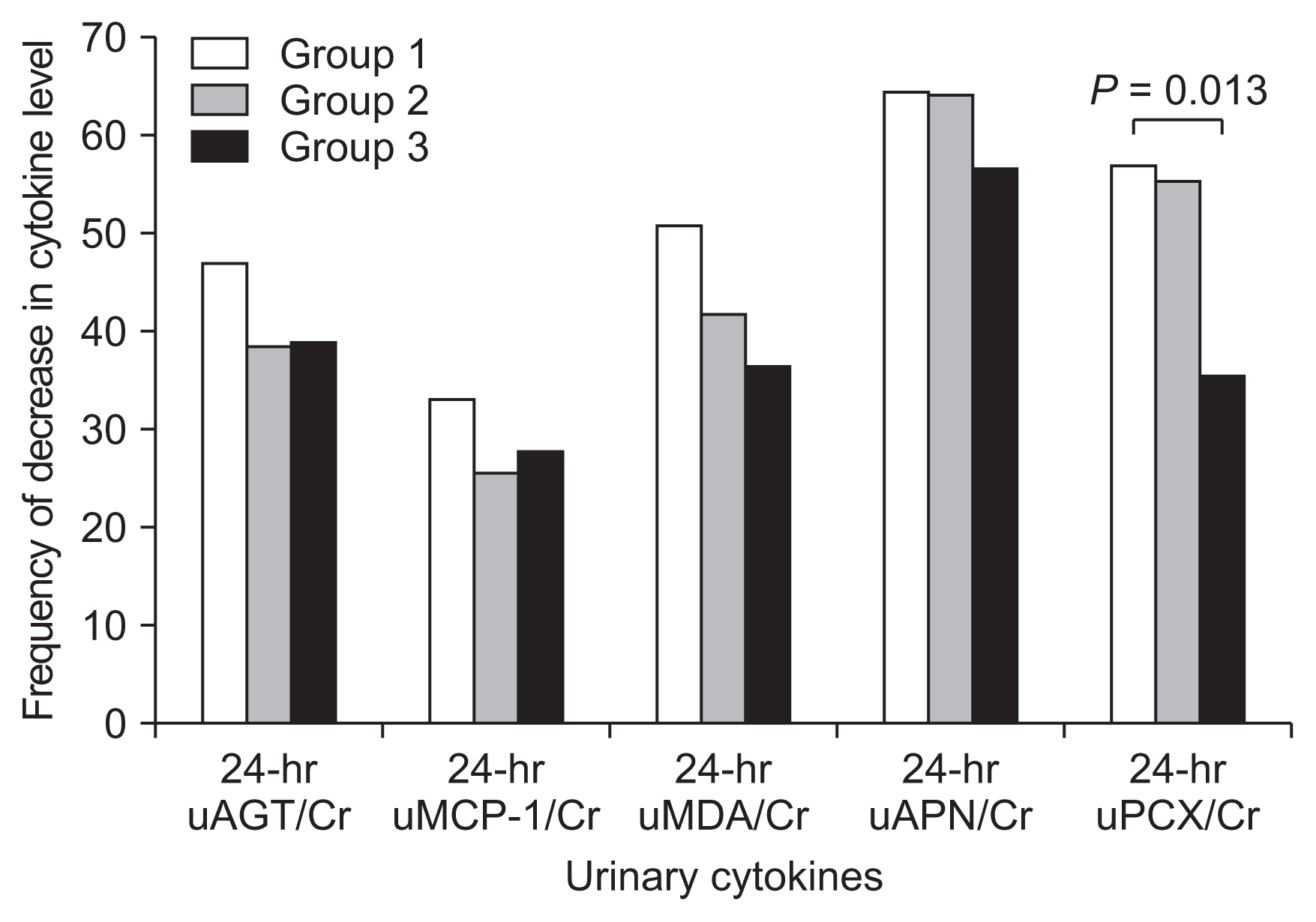
Changes in urinary cytokines according to change in body weight over 16 weeks
Frequency of decrease in cytokine level: The frequency of a 25% or greater reduction in 24-hour urinary cytokine to creatinine ratio at 16 weeks compared to 0 weeks. Group 1 (≥ 1.5% decrease in body weight), group 2 (1.5–0.1% decrease in body weight), and group 3 (≥ 0.0% increase in body weight).
AGT, angiotensinogen; APN, adiponectin; Cr, creatinine; MCP-1, monocyte chemoattractant protein-1; MDA, malondialdehyde; PCX, podocalyxin; u-, urine.
Discussion
In this subanalysis, we demonstrate that even minimal unintentional weight reduction had additive effects on the anti-proteinuric effects of ARBs in hypertensive CKD patients. Over the study period, weight loss independently increased the probability of reduced albuminuria. Among the urinary cytokines evaluated to elucidate mechanisms, only podocalyxin was significantly decreased in participants who lost weight. Furthermore, both estimated urine albumin excretion at 0 weeks and the ratio of urine albumin excretion at 16 weeks compared to 0 weeks were independent risk factors for decreased urinary podocalyxin.
As mentioned above, many studies have explored the relationship between weight loss and CKD progression. Overweight and obese weight categories are known to lead to an increase in the incidence of diabetes and hypertension, which are independent risk factors for and the leading causes of ESRD [10,19–21]. Recently, obesity itself has been proposed as an independent risk factor for CKD and ESRD in several observational studies [10,22,23]. Lifestyle changes such as calorie- and salt controlled diets and regular exercise, which can lead to weight reduction, have been considered important management strategies for CKD [5,12]. In the clinical trial on which this study was based, participants were intensively or conventionally educated about low-salt diets. Some patients unintentionally lost weight during the study period. Even if the degree of weight loss was minimal, weight reduction showed an additive effect on the anti-proteinuric effects of ARBs in hypertensive CKD patients. There was no evidence that weight reduction during the study period was related to disease progression.
Being obese or overweight leads to alterations in renal hemodynamics characterized by increased glomerular filtration pressure and perfusion [24–26]. Obesity also augments sympathetic activity [27], activates the RAS [28,29], activates insulin resistance [30], increases inflammation and oxidative stress [31], and attenuates the bioactivity of nitric oxide [32,33]. Furthermore, levels of adipose tissue-derived adipokines, which influence podocyte biology, are altered in obese patients [34]. Adiponectin, an adipokine, is decreased in obese patients, and its levels can be normalized by weight reduction [35]. Based on this pathophysiology, the beneficial effects of weight reduction on renal damage induced by being overweight might be due to decreases in hyperfiltration, filtration pressure, inflammation, and oxidative stress, as well as increases in nitric oxide bioactivity and adiponectin level. Therefore, weight loss could effectively decrease proteinuria.
In this study, we measured urinary biomarkers such as AGT as an index of intrarenal RAS status, MDA as a marker of oxidative stress, MCP-1 as an index of inflammation status, adiponectin, and podocalyxin as a marker of podocyte injury. Among these urinary biomarkers, only podocalyxin significantly decreased with the percent change in body weight over 16 weeks (Fig. 3). Albuminuria also significantly decreased with the percent change in body weight (Fig. 2). Through this study, we observed a close relationship between unintentional weight loss and improved albuminuria and also between albuminuria and urinary podocalyxin excretion. Consequently, we suggest that weight loss reduces albuminuria as a result of improved glomerular injury by ameliorating podocyte damage.
Reduction in proteinuria is one of the most valuable treatments for CKD patients, and it is achieved by pharmacological and non-pharmacological management methods [36–38]. The results of this study, which showed an additive beneficial effect of unintentional weight reduction on treatment of albuminuria in non-obese and obese hypertensive CKD patients, are very meaningful. Weight loss had a significant additive effect on reduction in proteinuria, even if weight reduction during the study period was minimal. Low salt and protein restricted diets, as well as weight loss, are related to decreased proteinuria. However, we demonstrated that minimal weight reduction independently reduced proteinuria. In addition, the decreased proteinuria induced by weight loss was related to decreased podocyte damage.
This study also has some limitations. First, we used 24-hour urine specimens and measured body weight at a single time point for each follow-up visit. Urine excretion could be influenced by the dietary intake of patients at certain time points. Weight measurement was also influenced by the time of measurements, weight scale, and apparel. Because this was a multicenter outpatient-based study, weight scales were different for each institution, and the time at which weight was measured differed according to clinic visit. However, weight loss was associated with decreased proteinuria regardless of seasonal changes. Second, this study was not designed to explore the effects of dietary changes and weight loss on the anti-proteinuric effects of RAS blockers. Hence, there might be confounding factors that were not considered regardless of the multivariate analysis. In particular, we could not distinguish between a loss of volume and solid weight. Third, only one parameter was used for each signal of RAS, inflammation, reactive oxygen species, and podocyte injury, which reduces the accuracy for detecting signal in the kidney. Although urine parameters were standardized by urine creatinine levels to remove error induced by inappropriate urine collection, their accuracy could be affected by this error. Finally, urine samples were stored until the end of the study, and cytokines were measured 6 months after the first urine collection period. During this period, urine contents could have been altered in each sample, introducing an accuracy error.
In conclusion, this study demonstrated that weight loss had an additive effect on the anti-proteinuric effects of treatment with ARBs in nondiabetic hypertensive CKD patients, even though the degree of weight loss was minimal. Those effects were demonstrated in both obese and non-obese participants. Possible mechanisms are related to reduced podocyte damage. Based on these results, a well-designed clinical trial is needed to elucidate the effect of weight change on the prognosis of CKD patients.
Supplementary Information
Acknowledgments
This study was funded by Seoul National University Bundang Hospital (No. 02-2015-046).
Notes
Conflicts of interest
All authors have no conflicts of interest to declare.



