| Kidney Res Clin Pract > Volume 33(3); 2014 > Article |
|
Abstract
Background
Catheter-related exit site infection is a major risk factor for the development of peritonitis and can contribute to failure of treatment maintenance in peritoneal dialysis (PD) patients. Although povidone-iodine can be used for exit site care, the irritation induced by the local application of povidone-iodine could lead to secondary infection. Therefore, we evaluated the clinical effectiveness of normal saline compared with povidone-iodine as a method of exit site care in chronic PD patients.
Methods
In all, 126 patients undergoing PD treatment for>6 months between January 2006 and December 2009 were enrolled. Data were retrospectively analyzed for the incidence of exit site infection and peritonitis for 2 years prior to and after December 2007. In addition, we identified the incidences of catheter-related infections during follow-ups from January 2010 to December 2013.
Results
The participantsū│ mean age was 58.8┬▒12.9 years. The incidences of exit site infection and peritonitis were one episode per 64.6 patientsŌĆōmonths and one episode per 40.4 patientsŌĆōmonths in the povidone-iodine group, respectively, whereas these were one episode per 57.5 patientsŌĆōmonths and one episode per 45.6 patientsŌĆōmonths in the normal saline group, respectively. Whereas Gram-positive bacteria most frequently caused catheter-related infections in both groups, culture-negative infections were dominant in the normal saline group.
Conclusion
Exit site care using normal saline did not increase the incidence of exit site infection and peritonitis. Therefore, normal saline may be an alternative treatment for exit site care in patients receiving PD.
Keywords
Catheter-related infections, Peritoneal dialysis, Peritonitis, Povidone-iodine, SalineChronic kidney disease (CKD) is recognized as a public health problem, and the number of patients with CKD treated with renal replacement treatment is increasing. A high rate of CKD is associated with the elevated prevalence of obesity, diabetes, hypertension, and increased number of elderly people [1], [2], [3]. Peritoneal dialysis (PD) is one of the major treatments for patients with end-stage renal disease (ESRD). In particular, PD is effective in patients affected by severe heart disease, such as heart failure [4].
Catheter-related infections are considered an important cause of morbidity in PD patients [5]. In addition, catheter-related exit site infection is a major risk factor for the development of peritonitis and can contribute to treatment failure in PD [6]. Prevention of catheter-related infections is a key to maintaining treatment with PD.
There are several protocols for exit site care. Some authors have proposed that prophylactic use of antibiotics to the nose or to the catheter exit site can reduce the incidence of catheter-related infections [7], [8]. Other studies have reported that the application of topical disinfectants such as povidone-iodine, water and nondisinfectant soap, or hydrogen peroxide have benefits in chronic exit site care [9], [10]. Povidone-iodine applied to the catheter exit site reduces the incidence of exit site-related infections, but the irritation induced by the local application of povidone-iodine could lead to secondary exit site infection [11], [12]. In addition, a recent report has suggested that normal saline is more beneficial than povidone-iodine for preventing exit site infections [4]. However, the question of whether solutions are more effective for preventing infection remains unclear.
In this study, we aim to identify differences in the incidences of peritonitis and exit site infection depending on the exit site care method in patients receiving PD.
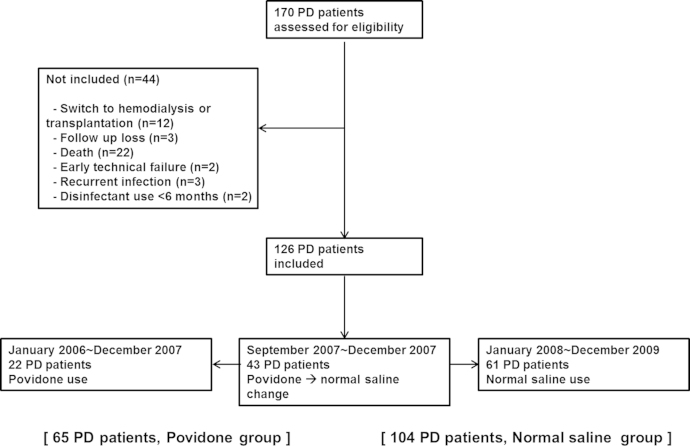
This study was conducted at Dong-A University Hospital, Busan, Republic of Korea. In our dialysis center, the exit site care method changed gradually from povidone-iodine to normal saline in September 2007, and almost all patients were treated with saline by December 2007. Therefore, we compared the incidences of exit site infection and peritonitis between exit site care using povidone-iodine from January 2006 to December 2007 and that using normal saline from January 2008 to December 2009 (Fig. 1). By December 2009, a total of 126 patients, including 22 patients using only povidone-iodine, 61 patients using only normal saline, and 43 patients who had changed from povidone-iodine to normal saline for exit site care, were enrolled. Among patients in whom the dressing method was changed, the patients who received dressings with povidone-iodine were included in the povidone-iodine group until the dressing method changed from povidone-iodine to normal saline.
If the dressing method was changed from povidone-iodine to normal saline, the patients were included in the normal saline group during dressing with normal saline. In December 2009, 104 patients were enrolled in the normal saline group, and 65 patients were enrolled in the povidone-iodine group. Participants were enrolled if they had maintained PD therapy for>6 months between January 1, 2006 and December 31, 2009. The criteria for exclusion included a switch to hemodialysis (HD), kidney transplantation, or death during the study; patients lost to follow-up because of transfer to another hospital; patients with suspected technical failure such as peritonitis or exit site infection within 6 months of starting PD; patients with repeated peritonitis or exit site infections within 2 months after previous catheter-related infections; or disinfectant use of<6 months.
Medical records were retrospectively analyzed for the method of PD, such as continuous ambulatory peritoneal dialysis (CAPD) or automated peritoneal dialysis, the type of dialysate, including Physioneal or Dianeal (all from Baxter Healthcare Corporation, Deerfield, IL, USA), the frequency of exit site dressing, and the use of tub baths. In addition, we identified the incidences of catheter-related infections during follow-ups from January 2010 to December 2013. During this interval, if inflammation was suspected, the method of dressing was temporarily changed from normal saline to povidone-iodine.
Catheter-related infections were defined as exit site infection and peritonitis. The exit site was assessed at least once a month by either a nephrologist or dialysis nurse. Exit site swab cultures from pericatheter skin were taken using sterile cotton-wool swabs when infection was suspected on the basis of erythema, swelling, induration, soreness, and tenderness at the exit site [11]. When peritonitis was suspected, peritoneal effluent cultures were performed. Peritonitis was diagnosed if the peritoneal fluid was cloudy, the effluent had a white blood cell count of>100/mm3, and at least 50% of the white blood cells were polymorphonuclear leukocytes [11].
The data are presented as mean┬▒SD (standard deviation) or frequency (count and percentage). The patientsū│ characteristics were analyzed using Student t test for continuous variables and the Chi-square test for categorical variables. The MannŌĆōWhitney U test analyzed the nonparametric data. All analyses were conducted using SPSS version 18.0 software (SPSS Inc., Chicago, IL, USA). A P value<0.05 was considered statistically significant.
The clinical characteristics are shown in Table 1. The mean age of the PD patients was 58.8┬▒12.9 years. Seventy (55.6%) of the total study population were male, and 98 (77.8%) patients were undergoing CAPD. The underlying causes of ESRD were diabetes mellitus in 75 (59.5%) patients, hypertension in 32 (25.4%) patients, and glomerulonephritis in nine (7.1%) patients.
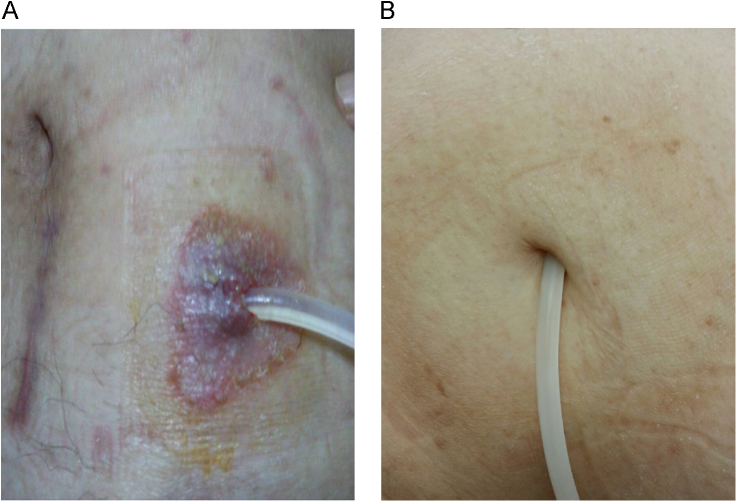
Images of exit sites dressed with povidone-iodine (A) or normal saline (B) are presented in Fig. 2. Sixty-five patients treated with povidone-iodine for exit site care were followed for a total of 1,615 patient-months (Table 2). In patients using povidone-iodine, the incidences of exit site infections and peritonitis were 25 (1 episode per 64.6 patients-months) and 40 (1 episode per 40.4 patients-months), respectively. One hundred and four patients who used normal saline for exit site care were followed for a total of 2,645 patient-months. Forty-six patients had exit site infections (1 episode per 57.5 patients-months), and 58 patients had peritonitis (1 episode per 45.6 patients-months). The differences in the incidences of exit site infections (P=0.636) or peritonitis (P=0.549) between dressing with povidone-iodine and normal saline were not statistically significant.
Of the participants using povidone-iodine (n=65), 20 (30.8%) experienced itching and 15 (23.1%) experienced skin irritation (Table 2). Among them, itching and skin irritation at the exit site alleviated in 21 (33.9%) patients after the dressing method was changed from povidone-iodine to normal saline. Of the participants using normal saline (n=104), 7 (6.7%) experienced side effects such as itching or skin irritation. There was a significant difference in the incidence of side effects between the povidone-iodine and normal saline groups (53.8% vs. 7%, P<0.001).
The etiologic organisms of catheter-related infections are listed in Table 3. Exit site infections and peritonitis were most often caused by Gram-positive bacteria. Catheter-related infections caused by Gram-negative bacteria occurred in 11 episodes in the povidone-iodine group and 14 episodes in the normal saline group. Culture-negative infections were found in 17 (16.3%) cases of peritonitis and nine (8.6%) cases of exit site infection in the normal saline group and four (6.2%) cases of peritonitis in the povidone-iodine group; we found no evidence of culture-negative exit site infections in this group. Culture-negative infections, especially in cases of exit site infection, were dominant in the normal saline group compared with the povidone-iodine group (P=0.019). Chronic exit site care using normal saline did not increase the incidences of exit site infection and peritonitis compared with care using povidone-iodine; however, the normal saline group had a higher incidence of culture-negative exit site infections.
A total of 104 patients were followed up from January 2010 to December 2013 for a total of 3,153 patient-months (Table 4). The incidences of exit site infection and peritonitis were 53 (1 episode per 59.5 patients-months) and 58 (1 episode per 54.4 patients-months), respectively. Compared with the previous result as shown in Table 2, the rate of exit site infection was similar, but the rate of peritonitis was lower in patients for whom the mode of dressing was changed than in those for whom normal saline alone was used. However, there was no significant difference in the incidences of exit site infections (P=0.865) or peritonitis (P=0.339) compared with the previous result. During the follow-up, 18 (17.3%) patients changed the type of renal replacement treatment due to recurrent peritonitis (data are not shown).
In this study, we found that exit site infection and peritonitis were not significantly associated with the methods of dressing, but the incidences of side effects such as skin irritation and itching were significantly lower in patients treated with normal saline than in those treated with povidone-iodine. This result seems to corroborate that of a recent study completed in Turkey, in which normal saline use for exit site care was not inferior to povidone-iodine use with regard to peritonitis and is in fact superior to povidone-iodine with regard to exit site infection in children receiving PD [4]. The current study is the first study to evaluate the clinical implications of dressing with normal saline for exit site care in Korea.
Patients using either normal saline or povidone-iodine had similar rates of peritonitis and exit site infections in this study. Regardless of the method of exit site care, Staphylococcus was the primary source of both exit site infection and peritonitis. This result may be explained as the nasal carrier of Staphylococcus is a high risk of exit site infection compared with no nasal carrier [15]. The question of how normal saline prevented catheter-related infections remains unanswered. In this study, the incidence of side effects such as itching and skin irritation increased when povidone-iodine was applied, but these incidences decreased after normal saline was used. Based on this result, one possible explanation is that normal saline may minimize skin stimulation and thus, decrease skin infections [12], [16]. Skin irritation may represent erythema at the exit site. Previous studies have reported that erythema alone at the exit site can be an indicator of exit site infections and peritonitis, subsequently requiring catheter removal [17]. In particular, Staphylococcus is the main organism found in erythematous exit site infections. In our study, dressing with povidone-iodine showed an elevated risk of skin irritation compared with that of normal saline. Therefore, dressing with normal saline is effective in patients with routine exit site care without signs of infection.
Despite many improvements in culture techniques, negative cultures account for 5ŌĆō33% of catheter-related infections [18], [19]. In this study, the incidence of culture-negative infections was 30 (24%). It is difficult to identify why these infections were culture negative, but reasons could include a history of recent antibiotic therapy, invalid sample collection, insufficient bacterial count, and complex bacterial characteristics. Previous studies have suggested that negative cultures are largely indicative of infections with coagulase-negative Staphylococcus. Povidone-iodine can eliminate viable bacteria from the skin and is likely to contain bactericidal activity against Staphylococcus
[20]. Therefore, povidone-iodine could be used as an antiseptic for exit site care, although it is cytotoxic and will delay exit site healing. In the present study, the frequency of culture-negative catheter-related infections was higher in the normal saline group than the povidone-iodine group, but there was no statistically significant association. On the basis of these results, we recommended that if an exit site infection is suspected, the method of dressing should be temporarily changed from normal saline to povidone-iodine until signs of infection are eliminated. As a result, the incidence of peritonitis reduced in the povidone-iodine with normal saline group compared with that in the normal saline alone group, although the difference in this incidence was not statistically significant. In addition, 18 (17.3%) patients in this study were transferred to HD due to recurrent peritonitis during the follow-up. In studies from Scotland, 42.2% patients were transferred to HD during the 3.5-year follow-up period [21]. In addition, recurrent peritonitis was associated with a high rate of catheter removal (37%) in studies from Australia and New Zealand [22]. Compared with previous studies, our study did not show such a high rate of transfer to HD. Therefore, if inflammation is suspected, povidone-iodine may be recommended.
This study has some limitations. Firstly, as this study was a retrospective analysis, certain factors such as the method of catheter insertion and the use of prophylactic antibiotics, including the topical application of mupirocin or gentamicin, were not controlled. However, prophylactic antibiotics were not routinely used for the periods of investigation in our center. Secondly, because we excluded patients who had experienced recurrent events within 2 months from previous catheter-related infections, the incidences of events may have been underreported. Thirdly, because the number of included patients was small, the power of the study was limited. Lastly, from September 2007 to December 2007, the exit site care method changed from povidone-iodine to normal saline. During this period, it is ambiguous to reflect what kind of disinfectant is associated with catheter-related infections.
In this study, it was shown that exit site care using normal saline was not inferior compared with exit site care using povidone-iodine. Exit site care with normal saline was superior to treatment with povidone-iodine with regard to side effects. The transient application of povidone-iodine may provide benefits in patients with signs of inflammation. In conclusion, dressing with normal saline may act as an alternative method for the prevention of catheter-related exit site infections in patients receiving PD. Further comparative studies are needed to explain the efficacy of normal saline in the prevention of catheter-related exit site infections in patients with PD. Studies are also required to reduce the incidence of Gram-negative infection in this group.
References
1. Mokdad AH, Ford ES, Bowman BA, Dietz WH, Vinicor F, Bales VS, Marks JS. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA 289:2003;76ŌĆō79.


2. Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988ŌĆō2000. JAMA 290:2003;199ŌĆō206.


3. Glassock RJ, Winearls C. Ageing and the glomerular filtration rate: truths and consequences. Trans Am Clin Climatol Assoc 120:2009;419ŌĆō428.


4. Yavascan O, Anil M, Kara OD, Bal A, Akcan N, Senturk S, Unturk S, Aksu N. The comparison of exit-site care with normal saline and povidone-iodine in preventing exit-site infection and peritonitis in children on chronic peritoneal dialysis treatment. Saudi J Kidney Dis Transpl 22:2011;931ŌĆō934.

5. Piraino B. Dialysis: The importance of peritoneal catheter exit-site care. Nat Rev Nephrol 6:2010;259ŌĆō260.


6. Mahaldar A, Weisz M, Kathuria P. Comparison of gentamicin and mupirocin in the prevention of exit-site infection and peritonitis in peritoneal dialysis. Adv Perit Dial 25:2009;56ŌĆō59.

7. Bending M. Nasal mupirocin prevents Staphylococcus aureus exit-site infection during peritoneal dialysis. Mupirocin Study Group. J Am Soc Nephrol 7:1996;2403ŌĆō2408.


8. Bernardini J, Bender F, Florio T, Sloand J, Palmmontalbano L, Fried L, Piraino B. Randomized, double-blind trial of antibiotic exit site cream for prevention of exit site infection in peritoneal dialysis patients. J Am Soc Nephrol 16:2005;539ŌĆō545.


9. Luzar MA, Brown CB, Balf D, Hill L, Issad B, Monnier B, Moulart J, Sabatier JC, Wauquier JP, Peluso F. Exit-site care and exit-site infection in continuous ambulatory peritoneal dialysis (CAPD): results of a randomized multicenter trial. Perit Dial Int 10:1990;25ŌĆō29.

10. Strippoli GF, Tong A, Johnson D, Schena FP, Craig JC. Antimicrobial agents to prevent peritonitis in peritoneal dialysis: a systematic review of randomized controlled trials. Am J Kidney Dis 44:2004;591ŌĆō603.


11. Warady BA, Bakkaloglu S, Newland J, Cantwell M, Verrina E, Neu A, Chadha V, Yap HK, Schaefer F. Consensus guidelines for the prevention and treatment of catheter-related infections and peritonitis in pediatric patients receiving peritoneal dialysis: 2012 update. Perit Dial Int 32(Suppl 2):2012;S32ŌĆōS86.



12. Berns JS, Tokars JI. Preventing bacterial infections and antimicrobial resistance in dialysis patients. Am J Kidney Dis 40:2002;886ŌĆō898.


13. Lachapelle JM. Allergic contact dermatitis from povidone-iodine: a re-evaluation study. Contact Dermatitis 52:2005;9ŌĆō10.


15. Davies SJ, Ogg CS, Cameron JS, Poston S, Noble WC. Staphylococcus aureus nasal carriage, exit-site infection and catheter loss in patients treated with continuous ambulatory peritoneal dialysis (CAPD). Perit Dial Int 9:1989;61ŌĆō64.


16. Oduwole KO, Glynn AA, Molony DC, Murray D, Rowe S, Holland LM, McCormack DJ, Oū│Gara JP. Anti-biofilm activity of subinhibitory povidone-iodine concentrations against Staphylococcus epidermidis and Staphylococcus aureus. J Orthop Res 28:2010;1252ŌĆō1256.


17. Gonthier D, Bernardini J, Holley JL, Piraino B. Erythema: does it indicate infection in a peritoneal catheter exit site? Adv Perit Dial 8:1992;230ŌĆō233.

18. Holley JL, Moss AH. A prospective evaluation of blood culture versus standard plate techniques for diagnosing peritonitis in continuous ambulatory peritoneal dialysis. Am J Kidney Dis 13:1989;184ŌĆō188.


19. Kent JR, Almond MK. A survey of CAPD peritonitis management and outcomes in North and South Thames NHS regions (U.K.): support for the ISPD guidelines. International Society for Peritoneal Dialysis. Perit Dial Int 20:2000;301ŌĆō305.


20. Lacey RW. Antibacterial activity of povidone iodine towards non-sporing bacteria. J Appl Bacteriol 46:1979;443ŌĆō449.


Table┬Ā1
Clinical characteristics of study participants
Table┬Ā2
Incidence of catheter-related infections according to the protocol of exit site care
Table┬Ā3
Etiologic organisms of catheter-related infection
Table┬Ā4
Incidence of catheter-related infections during the follow-up
| Normal saline only (2,645 patients-months)ŌüÄ | Normal saline with povidone-iodine (3,153 patients-months)ŌĆĀ | P | |
|
|
|||
| Exit site infection | 0.865 | ||
| ┬ĀNumber of infections | 46 | 53 | |
| ┬ĀFrequency | 1/57.5 | 1/59.5 | |
| ┬Ā┬Ā(1 episode/patients-months) | |||
| Peritonitis | 0.339 | ||
| ┬ĀNumber of infections | 58 | 58 | |
| ┬ĀFrequency | 1/45.6 | 1/54.4 | |
| ┬Ā┬Ā(1 episode/patients-months) | |||



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print
















