Preliminary evaluation of the effect of revised reimbursement scheme in outpatient hemodialysis for medical aid recipients in Korea
Article information
Abstract
Background
South Korea has universal health coverage guaranteeing equitable healthcare for all. However, equity issues have been raised regarding hemodialysis reimbursement for medical aid recipients with chronic kidney disease. Physicians and civic groups demanded a revision of the discriminatory policy, and in response, the Ministry of Health and Welfare amended the hemodialysis case payment scheme. This study aims to evaluate the effectiveness of the reform and detect any unintended policy outcomes.
Methods
Data from the Health Insurance Review and Assessment Service of Korea was used. All subjects were patients with chronic kidney disease who received outpatient hemodialysis and medical aid from April 2017 to March 2022. The data was analyzed with descriptive statistics, and the generalized estimation equation was used to control for covariates and identify policy effects.
Results
The reform of the case payment scheme in 2021 raised the compensation level per hemodialysis case, which was fixed for 7 years from 2014, by approximately 2,000 Korean won. There was no negative effect such as additional expenditure resulting from an unintentional increase in medical use.
Conclusion
A year has passed since the implementation of the outpatient hemodialysis rate system reform for medical aid recipients. Our results indicate that the reform has gone smoothly, and we anticipate continuous efforts by the government to guarantee universal health coverage to medical aid recipients. Through such consistent endeavors to correct the discriminatory aspects of policies, South Korea will achieve true universal health coverage.
Introduction
South Korea is one of the countries that has achieved universal health coverage (UHC) guaranteeing equitable healthcare utilization for its entire population [1]. The Korean government has made it mandatory to enroll in the National Health Insurance Service (NHI), and approximately 97% of Koreans are NHI beneficiaries. The remaining 3% are medical assistance (MA) recipients who are unable to pay their insurance contributions. However, according to a recent study, the proportion of MA recipients among hemodialysis (HD) patients was higher (23.3%) than among the overall patient population. The criterion for receiving MA is not only low income but also severe illness [2]. Hence, it is surmised that because HD patients tend to face job and income loss after starting HD, their lowered income level and severe medical condition together make them eligible for MA [2]. Hence, a large proportion of HD patients are financially protected by the government.
However, equity issues have been raised regarding HD for MA chronic kidney disease (CKD) [3]. CKD is a disease in which the kidneys are in a state of damage for more than 3 consecutive months, leading to a continuous decline in renal function. Stages of CKD are classified based on the glomerular filtration rate, an indicator of renal function [4,5].
In Korea, the NHI reimburses fee-for-service (FFS) and provides MA with case payments (CP) to HD patients. The CP pays a fixed amount per HD case, and the amount rarely increases. Additionally, when a CP is claimed, it is impossible to claim for other medical services. CP for MA HD patients was implemented from 2001 and was revised in April 2021 [6–10]. Behind this rigorous standard, there is a concern that healthcare providers, in a bid to generate more revenue, could be tempted to push more services for HD patients who need to visit hospitals two to three times a week regularly.
Although the CP system is meaningful in preventing unnecessary expenditure and safeguarding the financial sustainability of MA, it contains the seeds of discrimination and stigma for MA recipients who need HD [11]. In this context, there have been several attempts to improve the CP scheme by loosening the constraints on prices and utilization. Healthcare providers and patient groups pointed out that CP made it difficult for MA recipients to receive medical services equivalent to those covered by the NHI.
In response to these concerns, in April 2021, the government revised its CP scheme [3]. They changed the fixed price amendable according to the results of contracts between providers and insurers, which aligns with how FFS works, with the intention to guarantee the right to health of MA dialysis patients. This means that the price of HD can continuously increase annually, similar to other medical services. Yet, there are concerns that this reform could trigger “unintended consequences.” Some scholars proclaim that as the price of medical services increases, medical providers could persuade patients to receive more services in order to maximize their own profits [12]. However, there is no empirical evidence of the unexpected consequences or even the positive aspects of the CP scheme reform.
Based on this context, the purpose of our study is to verify whether the CP scheme reform has achieved the objective of “improving the compensation” by alleviating the “restriction on a price rise.” Furthermore, this study aims to scrutinize and monitor whether the CP scheme reform has triggered inefficient expenditure due to unintended changes in HD utilization.
Methods
Ethics statement
This study was approved by the Institutional Review Board of the Health Insurance Review and Assessment Service (HIRA) and written informed consent from the subject was exempted because we used de-identified administrative data (No. X-2301-807-904).
Data source
This longitudinal study used claims and administrative data from the HIRA. All claims from the NHI and MA were collected by the HIRA. The claim statements of patients with CKD who visited healthcare providers for dialysis services between April 2017 and March 2022 were extracted. The claims statements for ambulatory MA dialysis patients are managed separately from other NHI claims using a unique computerized identifier (claim form code = ‘15’) and the costs of MA dialysis patients are reimbursed by the government under the CP scheme. On the other hand, HD for NHI patients is paid by insurers on the FFS basis identifier (claim form code = ‘03’).
Research subjects
The study population included CKD patients who visited medical institutions as outpatients and received dialysis services from April 2017 to March 2022. We selected MA recipients who had CKD disease codes (N18 in International Classification of Diseases, 10th Revision) and who had received HD services and defined them as analysis subjects according to the “2020 disease behavior calculation standards guide” published by the HIRA in Korea [13]. Patients of all ages who had medical claim records except the deceased were included in the analysis. We aggregated the use of medical services (visit days) and expenditures (medical expenses) of dialysis patients covered by MA. To analyze the effect of the CP scheme reform implemented on April 1, 2021, “1 year” of this study is operationally defined as “from April 1 to March 31.” However, for descriptive convenience, the period (1 year) was designated as the starting point. The year-wise breakup of number of subjects is as follows: 2017, 15,518 patients; 2018, 16,312 patients; 2019, 17,139 patients; 2020, 17,696 patients; and 2021, 18,832 patients.
Statistical methods
This study is primarily composed of two methods. Descriptive statistics were used for the total number of hospital visits per year, medical expenses, medical expenditures per visit, and number of patient visits per week. The generalized estimation equation (GEE) was used to conduct an in-depth analysis to determine whether the previously revealed changes under “the average expenditure per visit” and “the average number of visits per week” were statistically significantly different, even after controlling for sex, age, and regional characteristics. The GEE is a nonparametric method that is useful for analyzing repeatedly measured data and requires the assumption of the correlation of the error term. However, unlike the parameter estimation method, it has a unique characteristic in that the calculated coefficients refer to the “average effect” of the population group, not each individual [14]. To verify the effect of the CP scheme reform, all records of medical use for dialysis of MA recipients were converted to panel data, with each individual patient measured repeatedly. Therefore, it is reasonable to assume a correlation between errors when estimating the regression model, which justifies the application of the GEE method for this study. In total, 26,715 patients were analyzed using this model.
In this study, the number of subjects analyzed exceeded 85,000. It has been pointed out that the p-value of 0.05 is too generous for recent statistical studies and affects the reliability of the study [15]. As the number of observations was too large, the probability of significance would have been very small; hence, the critical value to verify statistical significance was adjusted strictly (conservatively) to 0.01% (p = 0.0001), not 5% (p = 0.05).
Results
Current situation
Fig. 1 shows the use of outpatient dialysis services by chronic renal failure (CRF) patients in Korea. The number of NHI-CKD outpatient dialysis patients increased from 52,738 in 2017 to 65,117 in 2021, an increase of 12,379 (23.5%). The number of MA-CRF patients increased by 3,314 (21.4%), from 15,518 in 2017 to 18,832 in 2021.
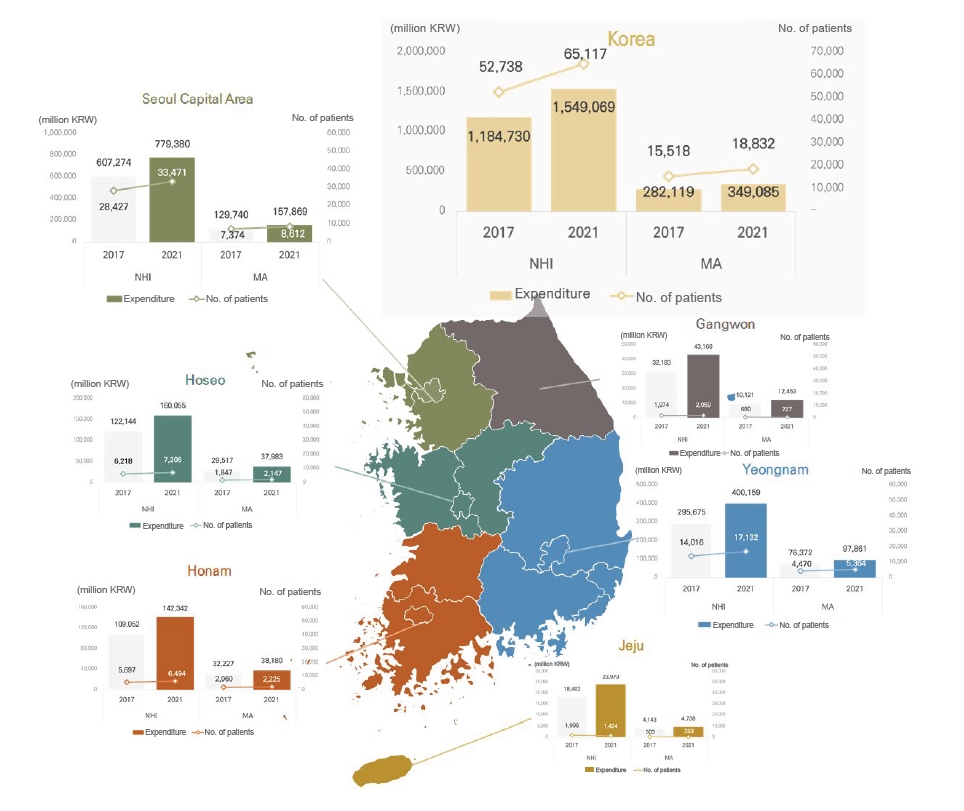
Number of patients and total amount of dialysis expenditure by region and insurer.
Bar charts show the total expenditure of National Health Insurance (NHI) and medical assistance (MA) hemodialysis (HD) patients and line graphs show the number of NHI and MA patients who received HD in Korea’s traditional six vast provinces. KRW, Korean won.
NHI-CKD outpatient dialysis service expenditure was KRW 1.55 trillion (about USD 1.3 billion), indicating a 30.8% increase from KRW 1.18 trillion (about USD 1.0 billion) in 2017. Medical expenditure for MA outpatient dialysis was KRW 349.1 billion (about USD 3.0 million) in 2021, compared to KRW 282.1 billion (about USD 228.9 million) in 2017, indicating an increase of only 23.7%. This difference can be interpreted as the difference between the NHI and CP systems.
Descriptive analysis on the effects of the case payments scheme reform
After the CP scheme reform in 2021, the average medical expenditure per visit of MA increased by about KRW 2,000, which was fixed at around KRW 146,000 (about USD 118.5) for 4 years from 2017 to 2020 (Fig. 2). In addition, the number of dialysis days was compared to identify unintended changes in medical utilization. The average number of dialysis days per week in 2021 was 2.42, a slight decrease from 2.45 in 2020 before the reform. However, from 2017 to 2019, before the reform was made, there was a slight but steady increase in number of dialysis days (Fig. 2). In contrast, the average number of visits per week decreased in 2021. Supplementary Table 1 includes the number of patients, number of visits, and healthcare costs for dialysis of MA patients stratified by year.
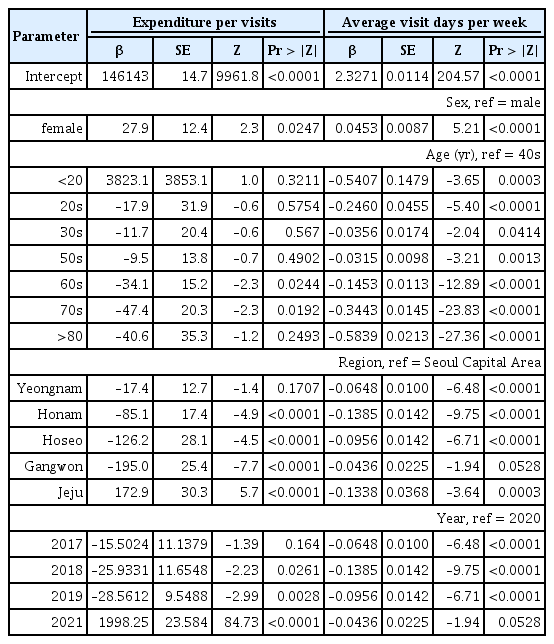
Unintended change in hemodialysis utilization and expenditure
The policy’s effect was examined after controlling for demographic factors such as sex, age, and region (Table 1). The average medical expenditure per patient visit in 2021, which empirically shows the expected effect of the CP scheme reform, increased by about 2,000 won on average compared to 2020 (β = 1,998.25, p < 0.0001). However, the average number of visits per week, which was analyzed to verify the unintended effect of the price increase, increased slightly in 2021 compared with that in 2020. However, these differences were under the range of as usual. This indicates that the CP scheme reform did not result in a dramatic change in the actual frequency of medical use.
While there was no statistically significant change in the average medical expenditure per visit by age group, the average number of visits differed slightly among age groups. Those in their 40s had the highest average number of visits per week, and there was a slight decrease in the younger and older age groups. In the 20s (β = –0.246, p < 0.0001), 60s (β = –0.1453, p < 0.0001), 70s (β = –0.3443, p < 0.0001), and 80s (β = –0.5893, p < 0.0001), the average number of days per week was significantly lower than 40s. For those under the 20s (β = –0.5407, p = 0.0003), in the 30s (β = –0.0356, p = 0.0414), and 50s (β = –0.0315, p = 0.0013), the average number of days per week was slightly lower on average.
The average medical expenditure per visit was lower in Honam, Hoseo, and Gangwon than in the Seoul Capital Area. On Jeju Island, the average medical expenditure per visit was slightly higher than that in the Seoul Capital Area. The average number of visits per week was significantly lower in Yeongnam and Honam than in the Seoul Capital Area. Gangwon and Jeju also had slightly fewer visits per week than the Seoul Capital Area, but this difference was not statistically significant.
On verifying the robustness of the coefficients after estimation, it was found that the coefficients of the period and regional variables in the average medical expenditure model and all variables in the model of the average visiting number were significant, reconfirming that they were influential variables in the model.
Discussion
This study aimed to confirm the effect of a CP scheme amendment on dialysis services for MA recipients and examine any unintended adverse effects. The analysis resulted in two main findings. First, the price, which had remained unchanged since 2014, increased by nearly KRW 2,000 after the reform. From 2021, the Korean government set prices for hospitals (1,315.22 score) and clinics (1,168.07 score) by referring to NHI’s resource based relative value scale for the price of MA HD and embracing medical examination fees, examination fees, essential oral medications, and hematopoietic agents. Thus, the price has risen by about KRW 2,000 and will continue to increase based on future health insurance price negotiations.
Second, by confirming that the revised compensation system had produced little change in the average number of dialysis days per week for MA recipients, the study showed that an increase in medical utilization and expenditure, which would be considered unintended adverse effects of the policy, had not occurred to a notable degree. However, this study demonstrated a statistical improvement in reimbursement for outpatient dialysis services under MA after the price rise under the CP scheme, marking the first increase in 7 years since 2014. Descriptive analysis results showed that the revision of the CP scheme, which aimed to maintain the average healthcare cost per visit constant, was effective until 2020, with changes beginning after the reform in 2021.
In 2001, the CP scheme for outpatient dialysis patients was first introduced to address concerns of the Korean government regarding the financial sustainability of MA financing, which is dependent on government budgets and competes with other national budgets [8]. However, under continuing inflation, the fixed pricing of the CP scheme was likely to cause a decline in the quality of dialysis services provided to MA recipients [9,16]. Nongovernmental organizations and the medical community expressed these concerns [7,10], and in 2021, the Korean government recognized the problem and implemented measures to allow continuous price increase in dialysis services in the future. As previously mentioned, most Korean medical services raise prices through contracts between healthcare providers and NHI, but MA outpatient dialysis was previously excluded. However, with the CP scheme reform of 2021, the MA outpatient dialysis service was also changed to allow for an annual price increase [3,17].
In addition, the fact that there was little change in medical utilization after the reform implies that the policy had no unintended adverse effects. The findings of the technical analysis of the reform’s effect contradict the a priori expectation that an increase in prices would lead to an increase in medical utilization and that suppliers would induce demand through CP revision. In other words, the relevance of the adverse effects of policy reform is limited. The analysis conducted in this study demonstrated that there was no change in medical utilization in response to variations in service prices, which can be attributed to the characteristics of the disease [8].
The adverse policy effect that economists fear may not occur because of the clinical characteristics of HD patients who require continuous medical use, but the actual amount of medical utilization is fixed at two to three times a week [8]. In other words, it can be assessed that the reform fulfilled its intended purpose without unintended negative effects. On the other hand, although the healthcare reimbursement system has improved in 2021, as shown in Fig. 1, there are still large differences in per-patient medical costs between MA and NHI. Eliminating such discriminatory restrictions remains an important task for the government.
This study has three limitations. The first pertains to the data used in the analysis. This study focused on a preliminary analysis of the effects of policy changes 1 year after the CP scheme reform. However, the data used for the analysis were limited to medical services provided between April 2021 and April 2022, the period when the policy was introduced. Hence, this short data period makes it challenging to evaluate the success of policy interventions. In addition, it was difficult to grasp changes in supplier behavior, such as labor costs other than medical use and drug cost reduction. To delicately confirm the negative effects of the policy, various studies using detailed analyses through surveys and various data should be conducted as follow-up studies.
The second limitation is that the study design focused only on the number of days of dialysis for patients with MA and did not consider other medical services. As mentioned previously, MA outpatients are allowed to obtain only dialysis services and are constrained from using other medical services. While this study suggests that CP scheme reform, which allows the price to be continuously adjusted, has had the intended and expected policy effects without adverse effects, it cannot provide evidence of the alleviation of the second restriction, namely the “restriction on other medical services.” Further research is needed to analyze not only the medical utilization of dialysis services but also the separate utilization of other services by dialysis patients.
The final limitation of this study is the difficulty in confirming changes in health outcomes such as mortality and complication rates of HD patients undergoing HD before and after the policy. However, this study could not consider this issue, as it aimed to conduct a timely statistical analysis only 1 year after the policy change to produce rapid evidence. We hope that future studies will fill this gap.
A year has passed since the reform of the MA outpatient HD rate system was implemented. The findings of this study indicate that the CP scheme reform was a step in the right direction and that continuous efforts to guarantee UHC to the MA will continue. By continuously working to improve policies that eliminate discriminatory practices, South Korea can achieve genuine UHC.
Supplementary Materials
Supplementary data are available at Kidney Research and Clinical Practice online (https://doi.org/10.23876/j.krcp.23.038).
Notes
Conflicts of interest
All authors have no conflicts of interest to declare.
Data sharing statement
The data presented in this study are available on request from the corresponding author.
Authors’ contributions
Conceptualization, Project administration: HK, JYL
Data curation: HK, YC, SK, KYJ
Formal analysis: HK, SK, KYJ
Methodology: HK, YC
Validation: DKR, HL
Visualization: HK
Writing–original draft: HK, DKR
Writing–review & editing: DKR, SK, HL, HL
All authors read and approved the final manuscript.