| Kidney Res Clin Pract > Epub ahead of print |
Abstract
Background
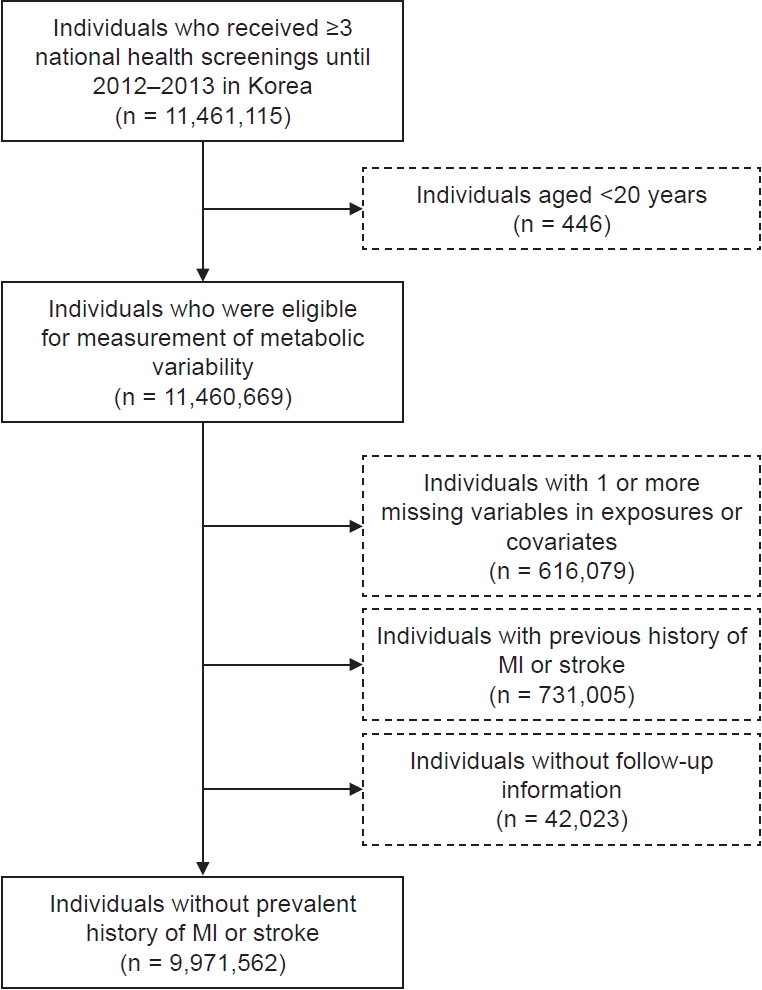
Methods
Results
Supplementary Materials
Notes
Funding
This research was supported by EverestMedicine Korea (No.0620234330). This research was supported by a 2022 Young Investigator Grant from the Korean Society of Nephrology. This research was supported by a grant funded by Seoul National University Hospital (grant number, 3020-210020).
Data sharing statement
The datasets used and/or analyzed in this study are available from the corresponding author on reasonable request.
AuthorsŌĆÖ contributions
Conceptualization, Methodology: JMC, KH, KWJ, SL, YK, SC, SGK, MK, EK, DKK, SP
Investigation: JMC, KH, KWJ, SL, YK, HH, EK, SP
Formal analysis: KWJ, DKK, SP, KH, JMC, SL, YK, SGK
Validation: DKK
Funding acquisition: DKK, SP
WritingŌĆōoriginal draft: All authors
WritingŌĆōreview & editing: All authors
All authors read and approved the final manuscript.
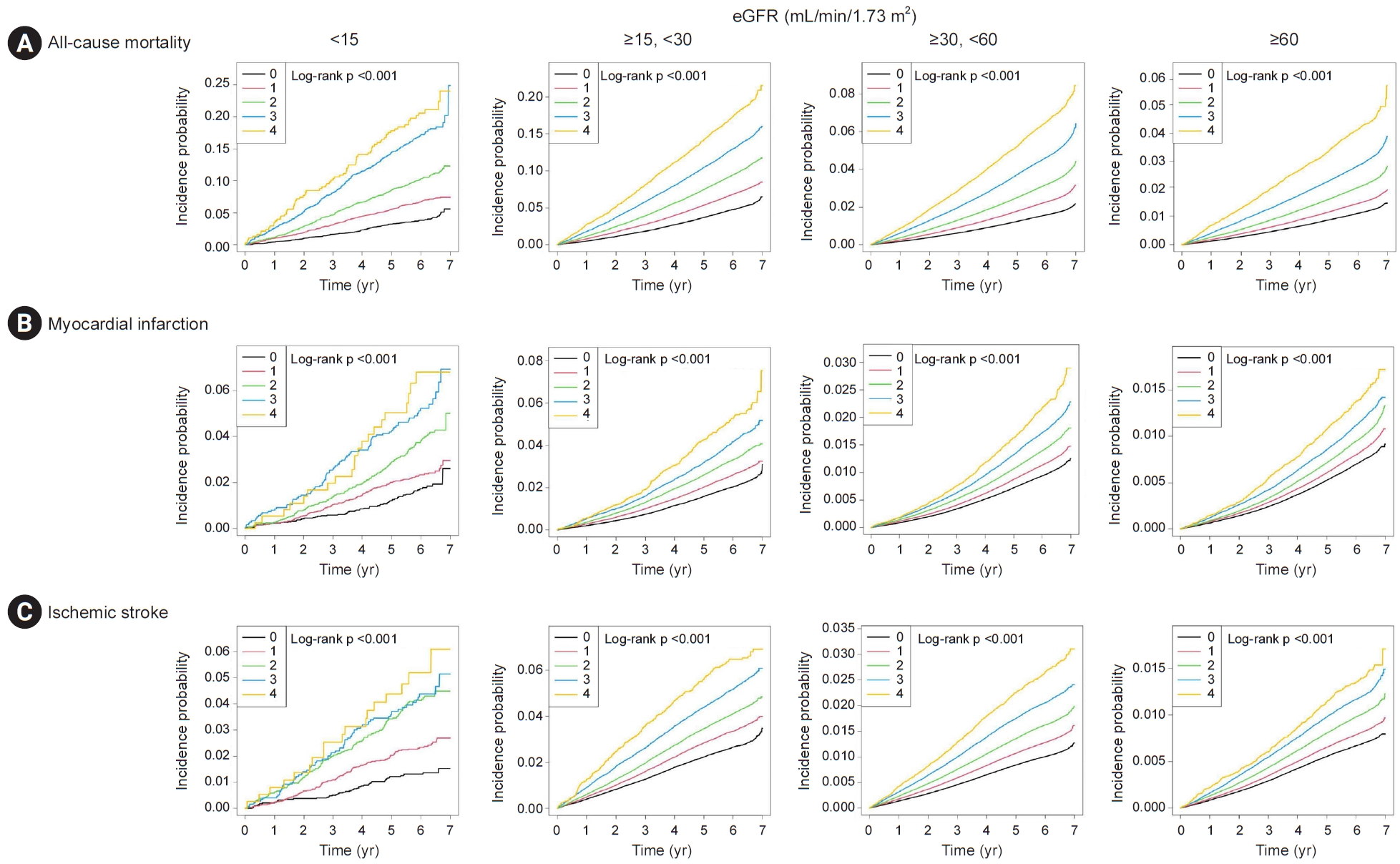
Figure┬Ā2.
Kaplan-Meier survival analysis curves according to the ranges of eGFR (<15, Ōēź15 to <30, Ōēź30 to <60, and Ōēź60 mL/min/1.73 m2).
Figure┬Ā3.
Hazard ratios according to the number of high-variability (Q4) metabolic parameters, stratified by baseline eGFR.

Table┬Ā1.
Data are expressed as number only, mean ┬▒ standard deviation, or number (%).
BMI, body mass index; BP, blood pressure; eGFR, estimated glomerular filtration rate; HDL, high-density lipoprotein; LDL, low-density lipoprotein; Q, quartile; VIM, variability independent of the mean.
The p-values were <0.001 for all variables due to the large size of the study population.
Table┬Ā2.
| eGFR category (mL/min/1.73 m2) | No. of high-variability (Q4) componentsa | No. of subjects |
Mortality |
MI |
Ischemic stroke |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of events | Incidence rateb | Age-sex adjusted model, aHR (95% CI) | p for interaction | Multivariable modelc, aHR (95% CI) | p for interaction | No. of events | Incidence rateb | Age-sex adjusted model, aHR (95% CI) | p for interaction | Multivariable model, aHR (95% CI) | p for interaction | No. of events | Incidence rateb | Age-sex adjusted model, aHR (95% CI) | p for interaction | Multivariable model, aHR (95% CI) | p for interaction | |||
| <15 | 0 | 3,777 | 152 | 6.78 | 1 (Reference) | <0.001 | 1 (Reference) | <0.001 | 65 | 2.91 | 1 (Reference) | <0.001 | 1 (Reference) | <0.001 | 50 | 2.91 | 1 (Reference) | <0.001 | 1 (Reference) | 0.002 |
| 1 | 5,469 | 370 | 11.57 | 1.48 (1.23ŌĆō1.79) | 1.42 (1.17ŌĆō1.71) | 126 | 3.97 | 1.26 (0.93ŌĆō-1.70) | 1.17 (0.87ŌĆō1.58) | 127 | 3.97 | 1.58 (1.14ŌĆō2.20) | 1.49 (1.07ŌĆō2.07) | |||||||
| 2 | 3,951 | 410 | 18.07 | 2.07 (1.72ŌĆō2.50) | 1.84 (1.53ŌĆō2.22) | 143 | 6.38 | 1.90 (1.41ŌĆō2.54) | 1.66 (1.24ŌĆō2.23) | 156 | 6.38 | 2.52 (1.83ŌĆō3.46) | 2.24 (1.63ŌĆō3.08) | |||||||
| 3 | 1,754 | 301 | 31.13 | 3.57 (2.94ŌĆō4.34) | 2.98 (2.45ŌĆō3.62) | 86 | 9.06 | 2.70 (1.96ŌĆō3.72) | 2.21 (1.60ŌĆō3.05) | 70 | 9.06 | 2.60 (1.81ŌĆō3.74) | 2.19 (1.52ŌĆō3.15) | |||||||
| 4 | 376 | 78 | 38.32 | 5.28 (4.02ŌĆō6.94) | 4.28 (3.26ŌĆō5.62) | 21 | 10.54 | 3.43 (2.10ŌĆō5.60) | 2.80 (1.72ŌĆō4.58) | 18 | 10.54 | 3.63 (2.12ŌĆō6.22) | 3.05 (1.78ŌĆō5.23) | |||||||
| Ōēź15, <30 | 0 | 93,993 | 4,543 | 8.19 | 1 (Reference) | 1 (Reference) | 1,911 | 3.47 | 1 (Reference) | 1 (Reference) | 2,471 | 3.47 | 1 (Reference) | 1 (Reference) | ||||||
| 1 | 137,861 | 9,556 | 11.85 | 1.32 (1.27ŌĆō1.37) | 1.26 (1.22ŌĆō1.30) | 3,512 | 4.39 | 1.19 (1.12ŌĆō1.26) | 1.12 (1.06ŌĆō1.18) | 4,545 | 4.39 | 1.16 (1.10ŌĆō1.21) | 1.10 (1.05ŌĆō1.15) | |||||||
| 2 | 91,721 | 8,820 | 16.62 | 1.71 (1.65ŌĆō1.77) | 1.55 (1.50ŌĆō1.61) | 2,956 | 5.64 | 1.45 (1.36ŌĆō1.53) | 1.29 (1.22ŌĆō1.36) | 3,649 | 5.64 | 1.31 (1.24ŌĆō1.38) | 1.19 (1.13ŌĆō1.25) | |||||||
| 3 | 33,060 | 4,351 | 23.15 | 2.24 (2.15ŌĆō2.34) | 1.91 (1.83ŌĆō1.99) | 1,297 | 7.00 | 1.72 (1.61ŌĆō1.85) | 1.46 (1.36ŌĆō1.56) | 1,643 | 7.00 | 1.57 (1.48ŌĆō1.67) | 1.36 (1.27ŌĆō1.44) | |||||||
| 4 | 5,428 | 958 | 31.78 | 2.99 (2.79ŌĆō3.20) | 2.41 (2.25ŌĆō2.58) | 265 | 8.94 | 2.17 (1.91ŌĆō2.46) | 1.76 (1.55ŌĆō2.00) | 325 | 8.94 | 1.88 (1.68ŌĆō2.12) | 1.56 (1.39ŌĆō1.75) | |||||||
| Ōēź30, <60 | 0 | 1,767,263 | 28,946 | 2.72 | 1 (Reference) | 1 (Reference) | 16,922 | 1.59 | 1 (Reference) | 1 (Reference) | 17,949 | 1.60 | 1 (Reference) | 1 (Reference) | ||||||
| 1 | 1,975,726 | 46,021 | 3.88 | 1.26 (1.25ŌĆō1.28) | 1.21 (1.19ŌĆō1.23) | 22,582 | 1.91 | 1.12 (1.10ŌĆō1.14) | 1.06 (1.04ŌĆō1.09) | 25,415 | 1.91 | 1.14 (1.12ŌĆō1.16) | 1.09 (1.07ŌĆō1.11) | |||||||
| 2 | 1,001,160 | 32,801 | 5.49 | 1.57 (1.54ŌĆō1.59) | 1.44 (1.41ŌĆō1.46) | 14,030 | 2.36 | 1.28 (1.25ŌĆō1.31) | 1.16 (1.14ŌĆō1.19) | 16,178 | 2.36 | 1.28 (1.25ŌĆō1.31) | 1.17 (1.15ŌĆō1.20) | |||||||
| 3 | 273,528 | 13,025 | 8.03 | 2.03 (1.99ŌĆō2.07) | 1.77 (1.74ŌĆō1.81) | 4,690 | 2.91 | 1.47 (1.42ŌĆō1.52) | 1.28 (1.23ŌĆō1.32) | 5,584 | 2.91 | 1.47 (1.42ŌĆō1.51) | 1.29 (1.25ŌĆō1.33) | |||||||
| 4 | 33,377 | 2,225 | 11.33 | 2.53 (2.42ŌĆō2.64) | 2.09 (2.00ŌĆō2.19) | 715 | 3.67 | 1.72 (1.60ŌĆō1.85) | 1.43 (1.33ŌĆō1.54) | 870 | 3.67 | 1.70 (1.59ŌĆō1.82) | 1.43 (1.34ŌĆō1.53) | |||||||
| Ōēź60 | 0 | 1,524,102 | 17,030 | 1.85 | 1 (Reference) | 1 (Reference) | 10,850 | 1.18 | 1 (Reference) | 1 (Reference) | 10,294 | 1.18 | 1 (Reference) | 1 (Reference) | ||||||
| 1 | 1,787,112 | 26,229 | 2.44 | 1.23 (1.20ŌĆō1.25) | 1.18 (1.16ŌĆō1.20) | 14,591 | 1.36 | 1.12 (1.09ŌĆō1.15) | 1.07 (1.05ŌĆō1.10) | 14,161 | 1.36 | 1.11 (1.08ŌĆō1.14) | 1.07 (1.04ŌĆō1.10) | |||||||
| 2 | 937,796 | 19,051 | 3.39 | 1.55 (1.52ŌĆō1.59) | 1.43 (1.40ŌĆō1.46) | 8,985 | 1.60 | 1.27 (1.23ŌĆō1.31) | 1.16 (1.13ŌĆō1.20) | 9,176 | 1.60 | 1.28 (1.25-1.32) | 1.19 (1.15ŌĆō1.22) | |||||||
| 3 | 261,973 | 7,355 | 4.70 | 1.96 (1.91ŌĆō2.01) | 1.72 (1.68ŌĆō1.77) | 2,953 | 1.89 | 1.44 (1.38ŌĆō1.50) | 1.27 (1.22ŌĆō1.32) | 3,066 | 1.89 | 1.43 (1.37ŌĆō1.49) | 1.27 (1.22ŌĆō1.33) | |||||||
| 4 | 32,135 | 1,309 | 6.85 | 2.55 (2.41ŌĆō2.69) | 2.12 (2.01ŌĆō2.25) | 440 | 2.32 | 1.66 (1.51ŌĆō1.82) | 1.41 (1.28ŌĆō1.55) | 435 | 2.32 | 1.52 (1.38ŌĆō1.67) | 1.30 (1.18ŌĆō1.43) | |||||||
Interactions by eGFR category on the association between metabolic variability and study outcomes were calculated in the multivariable models.
aHR, adjusted hazard ratio; CI, confidence interval; eGFR, estimated glomerular filtration rate; Q, quartile.
References
- TOOLS
-
METRICS

-
- 0 Crossref
- 0 Scopus
- 596 View
- 20 Download
- ORCID iDs
-
Jeong Min Cho

https://orcid.org/0000-0001-7643-994XKyungdo Han

https://orcid.org/0000-0002-9622-0643Kwon Wook Joo

https://orcid.org/0000-0001-9941-7858Soojin Lee

https://orcid.org/0000-0001-5633-3961Yaerim Kim

https://orcid.org/0000-0003-1596-1528Semin Cho

https://orcid.org/0000-0002-6060-9032Hyuk Huh

https://orcid.org/0000-0001-7608-0199Seong Geun Kim

https://orcid.org/0000-0002-8831-9838Minsang Kim

https://orcid.org/0000-0002-7949-0764Eunjeong Kang

https://orcid.org/0000-0002-2191-2784Dong Ki Kim

https://orcid.org/0000-0002-5195-7852Sehoon Park

https://orcid.org/0000-0002-4221-2453 - Related articles



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Supplement table 1
Supplement table 1 Print
Print















