1. Xu X, Nie S, Ding H, Hou FF. Environmental pollution and kidney diseases.
Nat Rev Nephrol 2018;14:313–324.



2. Perlman RL, Finkelstein FO, Liu L, et al. Quality of life in chronic kidney disease (CKD): a cross-sectional analysis in the Renal Research Institute-CKD study.
Am J Kidney Dis 2005;45:658–666.


3. Lee W, Wu X, Heo S, et al. Air pollution and acute kidney injury in the U.S. medicare population: a longitudinal cohort study.
Environ Health Perspect 2023;131:47008.


4. GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019.
Lancet 2020;396:1204–1222.


5. Registry Committee, Korean Society of Nephrology (KSN). Numerical overview of chronic kidney disease (CKD) in South Korea. KSN NEWS 2018;11:5.
6. Centers for Disease Control and Prevention. Chronic kidney disease in the United States, 2021. US Department of Health and Human Services, Centers for Disease Control and Prevention; 2021.
7. United States Renal Data System. 2020 USRDS Annual Data Report: epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2020.
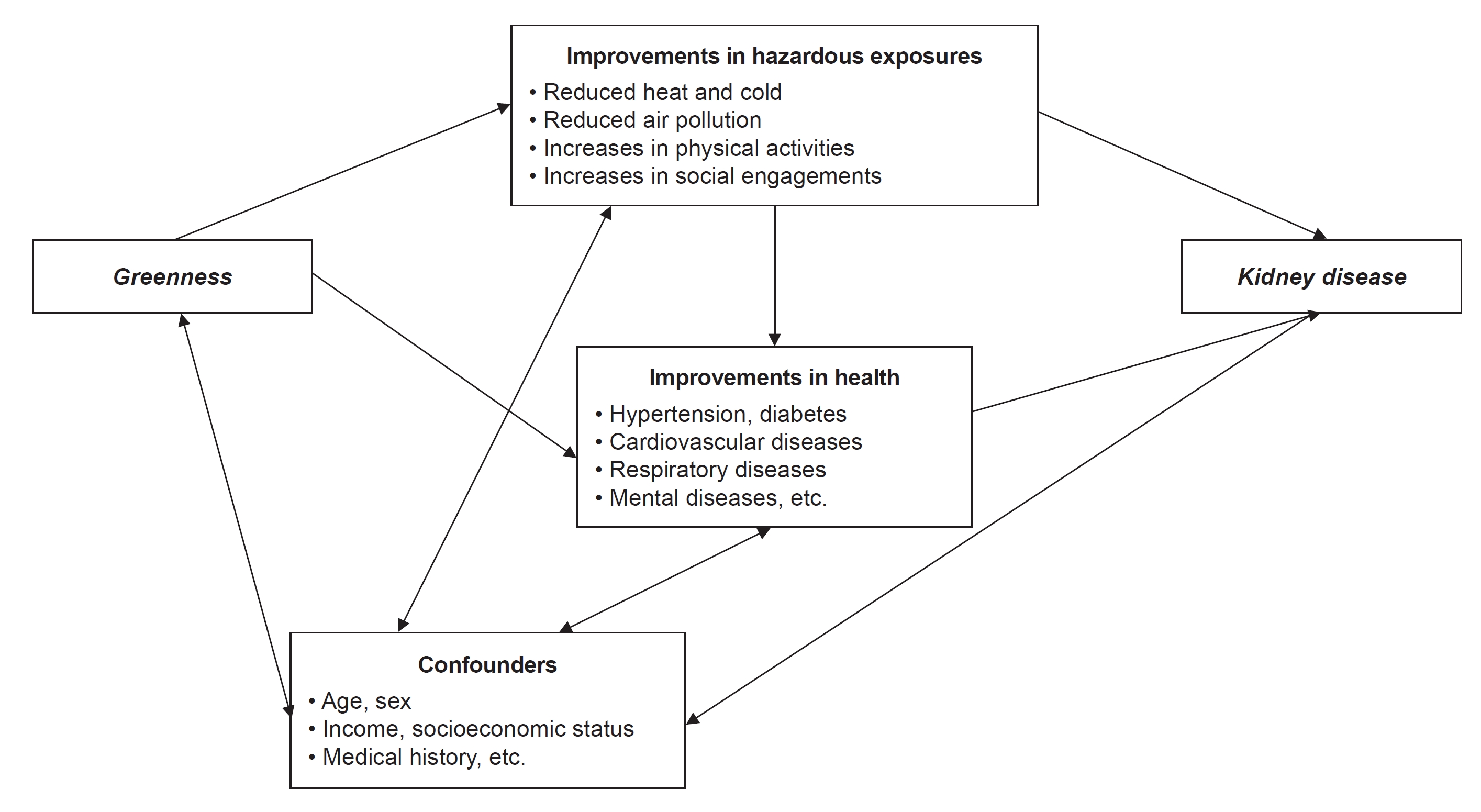
8. Markevych I, Schoierer J, Hartig T, et al. Exploring pathways linking greenspace to health: theoretical and methodological guidance.
Environ Res 2017;158:301–317.


9. Lee AC, Maheswaran R. The health benefits of urban green spaces: a review of the evidence.
J Public Health (Oxf) 2011;33:212–222.


10. Bodicoat DH, O’Donovan G, Dalton AM, et al. The association between neighbourhood greenspace and type 2 diabetes in a large cross-sectional study.
BMJ Open 2014;4:e006076.



12. Villeneuve PJ, Jerrett M, Su JG, et al. A cohort study relating urban green space with mortality in Ontario, Canada.
Environ Res 2012;115:51–58.


13. Tallis M, Taylor G, Sinnett D, Freer-Smith P. Estimating the removal of atmospheric particulate pollution by the urban tree canopy of London, under current and future environments.
Landsc Urban Plan 2011;103:129–138.

14. Son JY, Lane KJ, Lee JT, Bell ML. Urban vegetation and heat-related mortality in Seoul, Korea.
Environ Res 2016;151:728–733.



15. Lee W, Wu X, Heo S, et al. Associations between long term air pollution exposure and first hospital admission for kidney and total urinary system diseases in the US Medicare population: nationwide longitudinal cohort study.
BMJ Med 2022;1:e000009.



16. Lee W, Prifti K, Kim H, et al. Short-term exposure to air pollution and attributable risk of kidney diseases: a nationwide time-series study.
Epidemiology 2022;33:17–24.

17. Bowe B, Xie Y, Li T, Yan Y, Xian H, Al-Aly Z. Associations of ambient coarse particulate matter, nitrogen dioxide, and carbon monoxide with the risk of kidney disease: a cohort study.
Lancet Planet Health 2017;1:e267–e276.


18. Bowe B, Xie Y, Li T, Yan Y, Xian H, Al-Aly Z. Particulate matter air pollution and the risk of incident CKD and progression to ESRD.
J Am Soc Nephrol 2018;29:218–230.


19. Lee W, Heo S, Stewart R, et al. Associations between greenness and kidney disease in Massachusetts: the US Medicare longitudinal cohort study.
Environ Int 2023;173:107844.


20. Gessesse AA, Melesse AM. Chapter 8 - Temporal relationships between time series CHIRPS-rainfall estimation and eMODIS-NDVI satellite images in Amhara Region, Ethiopia. In: Melesse AA, Abtew W, Senay G, Extreme hydrology and climate variability. Elsevier; 2019. p. 81–92.
21. Fensholt R. Earth observation of vegetation status in the Sahelian and Sudanian West Africa: comparison of Terra MODIS and NOAA AVHRR satellite data.
Int J Remote Sens 2004;25:1641–1659.

22. Testa S, Soudani K, Boschetti L, Mondino EB. MODIS-derived EVI, NDVI and WDRVI time series to estimate phenological metrics in French deciduous forests.
Int J Appl Earth Obs Geoinf 2018;64:132–144.

23. James P, Hart JE, Banay RF, Laden F. Exposure to greenness and mortality in a nationwide prospective cohort study of women.
Environ Health Perspect 2016;124:1344–1352.



24. Chien JW, Yang YR, Chen SY, Chang YJ, Chan CC. Urban open space is associated with better renal function of adult residents in New Taipei City.
Int J Environ Res Public Health 2019;16:2436.



26. Liang Z, Wang W, Yang C, et al. Residential greenness and prevalence of chronic kidney disease: findings from the China National Survey of Chronic Kidney Disease.
Sci Total Environ 2022;806:150628.


27. Chien JW, Wu C, Chan CC. Open space and adult’s chronic kidney disease, overweight and diabetes in the metropolitan area of New Taipei City.
J Formos Med Assoc 2022;121:1657–1667.


28. Paoin K, Pharino C, Vathesatogkit P, et al. Residential greenness and kidney function: a cohort study of Thai employees.
Health Place 2023;80:102993.


29. Finkelstein J, Joshi A, Hise MK. Association of physical activity and renal function in subjects with and without metabolic syndrome: a review of the Third National Health and Nutrition Examination Survey (NHANES III).
Am J Kidney Dis 2006;48:372–382.


30. Hawkins MS, Sevick MA, Richardson CR, Fried LF, Arena VC, Kriska AM. Association between physical activity and kidney function: National Health and Nutrition Examination Survey.
Med Sci Sports Exerc 2011;43:1457–1464.

31. Palmer S, Vecchio M, Craig JC, et al. Prevalence of depression in chronic kidney disease: systematic review and meta-analysis of observational studies.
Kidney Int 2013;84:179–191.


32. Sun S, Weinberger KR, Nori-Sarma A, et al. Ambient heat and risks of emergency department visits among adults in the United States: time stratified case crossover study.
BMJ 2021;375:e065653.



33. Kim E, Kim H, Kim YC, Lee JP. Association between extreme temperature and kidney disease in South Korea, 2003-2013: stratified by sex and age groups.
Sci Total Environ 2018;642:800–808.


34. Crouse DL, Pinault L, Balram A, et al. Complex relationships between greenness, air pollution, and mortality in a population-based Canadian cohort.
Environ Int 2019;128:292–300.


35. Sedgwick P. Ecological studies: advantages and disadvantages.
BMJ 2014;348:g2979.


36. Lee W, Choi M, Bell ML, et al. Effects of urbanization on vulnerability to heat-related mortality in urban and rural areas in South Korea: a nationwide district-level time-series study.
Int J Epidemiol 2022;51:111–121.



37. Lim YH, So R, Lee C, et al. Ambient temperature and hospital admissions for acute kidney injury: a time-series analysis.
Sci Total Environ 2018;616-617:1134–1138.


38. Plataki M, Kashani K, Cabello-Garza J, et al. Predictors of acute kidney injury in septic shock patients: an observational cohort study.
Clin J Am Soc Nephrol 2011;6:1744–1751.

39. Bobb JF, Obermeyer Z, Wang Y, Dominici F. Cause-specific risk of hospital admission related to extreme heat in older adults.
JAMA 2014;312:2659–2667.



40. Lee W, Kim H, Choi HM, et al. Urban environments and COVID-19 in three Eastern states of the United States.
Sci Total Environ 2021;779:146334.



41. Mitchell RJ, Richardson EA, Shortt NK, Pearce JR. Neighborhood environments and socioeconomic inequalities in mental well-being.
Am J Prev Med 2015;49:80–84.


42. Casey JA, James P, Cushing L, Jesdale BM, Morello-Frosch R. Race, ethnicity, income concentration and 10-year change in urban greenness in the United States.
Int J Environ Res Public Health 2017;14:1546.



43. Jang J, Lee W, Choi M, Kang C, Kim H. Roles of urban heat anomaly and land-use/land-cover on the heat-related mortality in the national capital region of South Korea: a multi-districts time-series study.
Environ Int 2020;145:106127.


44. Lee W, Ebi KL, Kim Y, et al. Heat-mortality risk and the population concentration of metropolitan areas in Japan: a nationwide time-series study.
Int J Epidemiol 2021;50:602–612.



45. Barraclough KA, Agar JWM. Green nephrology.
Nat Rev Nephrol 2020;16:257–268.










 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print















