1. Mills KT, Bundy JD, Kelly TN, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries.
Circulation 2016;134:441ŌĆō450.



2. Bakris GL, Williams M, Dworkin L, et al. Preserving renal function in adults with hypertension and diabetes: a consensus approach. National Kidney Foundation Hypertension and Diabetes Executive Committees Working Group.
Am J Kidney Dis 2000;36:646ŌĆō661.

3. Saran R, Robinson B, Abbott KC, et al. US renal data system 2018 annual data report: epidemiology of kidney disease in the United States.
Am J Kidney Dis 2019;73:A7ŌĆōA8.


4. Hansson L, Zanchetti A, Carruthers SG, et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study Group.
Lancet 1998;351:1755ŌĆō1762.

5. Heart Outcomes Prevention Evaluation Study Investigators, Yusuf S, Sleight P, et al. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients.
N Engl J Med 2000;342:145ŌĆō153.


6. Beddhu S, Rocco MV, Toto R, et al. Effects of intensive systolic blood pressure control on kidney and cardiovascular outcomes in persons without kidney disease: a secondary analysis of a randomized trial.
Ann Intern Med 2017;167:375ŌĆō383.



7. Cheung AK, Rahman M, Reboussin DM, et al. Effects of intensive BP control in CKD.
J Am Soc Nephrol 2017;28:2812ŌĆō2823.



8. Klahr S, Levey AS, Beck GJ, et al. The effects of dietary protein restriction and blood-pressure control on the progression of chronic renal disease. Modification of Diet in Renal Disease Study Group.
N Engl J Med 1994;330:877ŌĆō884.


9. Wright JT Jr, Bakris G, Greene T, et al. Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: results from the AASK trial.
JAMA 2002;288:2421ŌĆō2431.


10. Ruggenenti P, Perna A, Loriga G, et al. Blood-pressure control for renoprotection in patients with non-diabetic chronic renal disease (REIN-2): multicentre, randomised controlled trial.
Lancet 2005;365:939ŌĆō946.


11. Brenner BM, Cooper ME, de Zeeuw D, et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy.
N Engl J Med 2001;345:861ŌĆō869.


12. Dekker FW, de Mutsert R, van Dijk PC, Zoccali C, Jager KJ. Survival analysis: time-dependent effects and time-varying risk factors.
Kidney Int 2008;74:994ŌĆō997.


13. Cole SR, Hern├Īn MA. Constructing inverse probability weights for marginal structural models.
Am J Epidemiol 2008;168:656ŌĆō664.



14. Xie D, Yang W, Jepson C, et al. Statistical methods for modeling time-updated exposures in cohort studies of chronic kidney disease.
Clin J Am Soc Nephrol 2017;12:1892ŌĆō1899.



15. Robins JM, Hern├Īn MA, Brumback B. Marginal structural models and causal inference in epidemiology.
Epidemiology 2000;11:550ŌĆō560.


16. Chang TI, Lim H, Park CH, et al. Associations of systolic blood pressure with incident CKD G3-G5: a cohort study of South Korean adults.
Am J Kidney Dis 2020;76:224ŌĆō232.


17. Appel LJ, Wright JT Jr, Greene T, et al. Intensive blood-pressure control in hypertensive chronic kidney disease.
N Engl J Med 2010;363:918ŌĆō929.



18. Ku E, Gassman J, Appel LJ, et al. BP control and long-term risk of ESRD and mortality.
J Am Soc Nephrol 2017;28:671ŌĆō677.


19. Sarnak MJ, Greene T, Wang X, et al. The effect of a lower target blood pressure on the progression of kidney disease: long-term follow-up of the modification of diet in renal disease study.
Ann Intern Med 2005;142:342ŌĆō351.


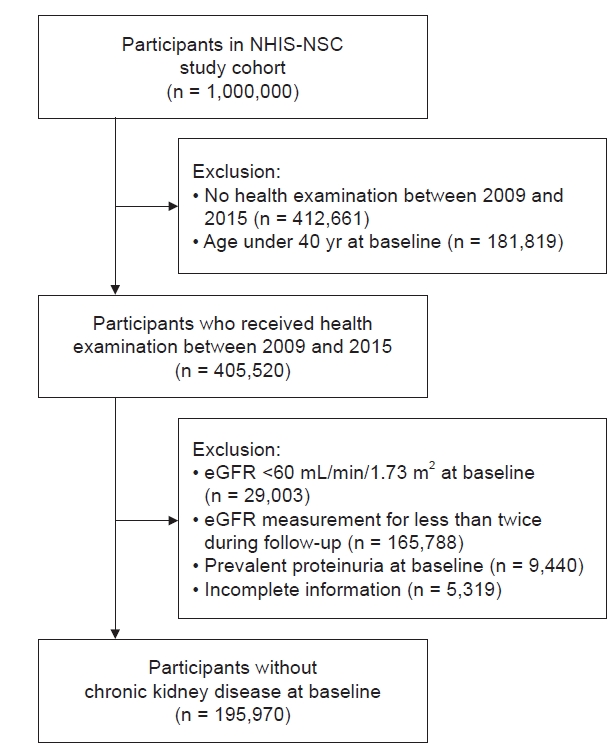
20. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: the National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea.
Int J Epidemiol 2017;46:e15.


21. Shin DW, Cho B, Guallar E. Korean National Health Insurance Database.
JAMA Intern Med 2016;176:138.

22. Seong SC, Kim YY, Park SK, et al. Cohort profile: the National Health Insurance Service-National Health Screening Cohort (NHIS-HEALS) in Korea.
BMJ Open 2017;7:e016640.



24. Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate.
Ann Intern Med 2009;150:604ŌĆō612.



25. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines.
J Am Coll Cardiol 2018;71:2199ŌĆō2269.

26. Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int 2013;3:1ŌĆō150.
27. Hern├Īn MA, Brumback BA, Robins JM. Estimating the causal effect of zidovudine on CD4 count with a marginal structural model for repeated measures.
Stat Med 2002;21:1689ŌĆō1709.


28. Lertdumrongluk P, Streja E, Rhee CM, et al. Dose of hemodialysis and survival: a marginal structural model analysis.
Am J Nephrol 2014;39:383ŌĆō391.



30. Anderson AH, Yang W, Townsend RR, et al. Time-updated systolic blood pressure and the progression of chronic kidney disease: a cohort study.
Ann Intern Med 2015;162:258ŌĆō265.



31. Doshi M, Streja E, Rhee CM, et al. Examining the robustness of the obesity paradox in maintenance hemodialysis patients: a marginal structural model analysis.
Nephrol Dial Transplant 2016;31:1310ŌĆō1319.


32. Hsu CY, McCulloch CE, Darbinian J, Go AS, Iribarren C. Elevated blood pressure and risk of end-stage renal disease in subjects without baseline kidney disease.
Arch Intern Med 2005;165:923ŌĆō928.


33. Reynolds K, Gu D, Muntner P, et al. A population-based, prospective study of blood pressure and risk for end-stage renal disease in China.
J Am Soc Nephrol 2007;18:1928ŌĆō1935.


34. Schaeffner ES, Kurth T, Bowman TS, Gelber RP, Gaziano JM. Blood pressure measures and risk of chronic kidney disease in men.
Nephrol Dial Transplant 2008;23:1246ŌĆō1251.


35. Jager KJ, Zoccali C, Macleod A, Dekker FW. Confounding: what it is and how to deal with it.
Kidney Int 2008;73:256ŌĆō260.


36. Wolfe RA, Strawderman RL. Logical and statistical fallacies in the use of Cox regression models.
Am J Kidney Dis 1996;27:124ŌĆō129.


37. Hern├Īn MA, Brumback B, Robins JM. Marginal structural models to estimate the causal effect of zidovudine on the survival of HIV-positive men.
Epidemiology 2000;11:561ŌĆō570.


39. Kidney Disease: Improving Global Outcomes (KDIGO) Blood Pressure Work Group. KDIGO 2021 clinical practice guideline for the management of blood pressure in chronic kidney disease.
Kidney Int 2021;99:S1ŌĆōS87.











 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Supplement table 1
Supplement table 1 Print
Print















