| Kidney Res Clin Pract > Volume 38(4); 2019 > Article |
|
Fitz-Hugh–Curtis syndrome (FHCS) is commonly associated with genital tract infection and presents as an inflammation and infection of the liver capsule. The clinical manifestation typically includes an acute onset of right upper quadrant (RUQ) abdominal pain. Computed tomography (CT) characteristically shows increased enhancement along the hepatic surface in the arterial phase and perihepatic fat stranding in the portal phase. We report an eccentric case of FHCS which unusually occurred after removal of a peritoneal catheter. A 59-year-old woman with diabetic nephropathy started automated peritoneal dialysis (APD) in 2015 because of end-stage kidney disease. While maintaining APD, she suffered from 3 episodes of peritonitis from 2015 to 2018.
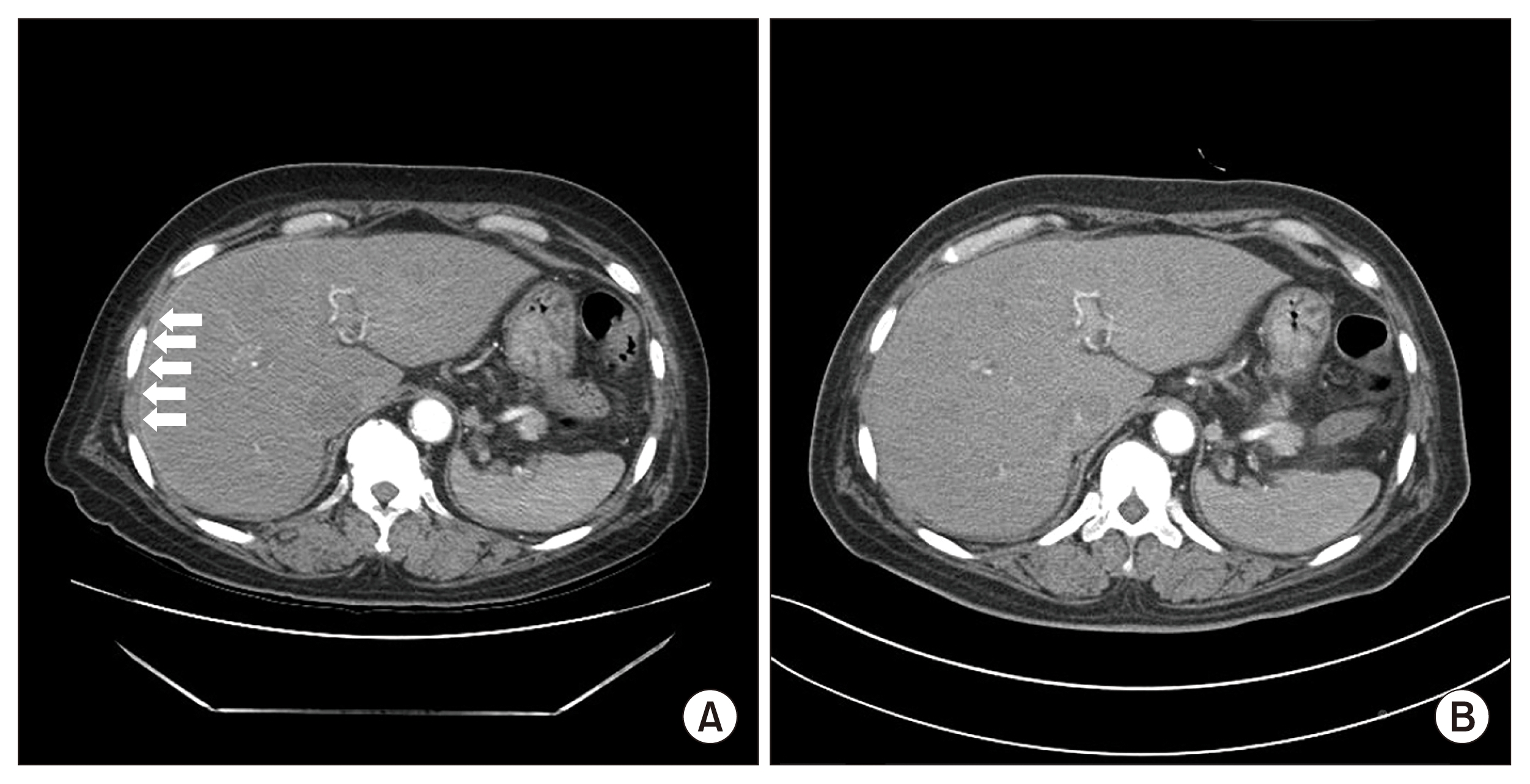
In April 2019, she was admitted via the emergency room due to symptoms of general weakness and dyspnea. Because her peritoneal dialysis (PD) was not effective in eliminating excessive fluid volume, the peritoneal catheter was removed by open surgical dissection; however, the catheter tip culture was not performed. Then the patient was converted to hemodialysis. Immediately after removal of the peritoneal catheter, the patient did not show any of the signs and symptoms of infection. Two months later, however, she complained of RUQ pain and fever. CT showed hepatic capsular enhancement in the arterial phase (Fig. 1A), suggestive of FHCS. Pelvic inflammatory disease was ruled out through gynecological examination, including polymerase chain reaction analyses for microorganisms associated with sexually transmitted diseases from a cervico-vaginal smear. After a three-week course of ceftazidime and azithromycin, her symptoms were resolved and CT findings of hepatic capsular enhancement completely disappeared (Fig. 1B).
It is well known that FHCS is a pathology complicated by pelvic inflammatory disease and usually occurs in young women of child-bearing age. However, a rare case of FHCS consequent to a post-operative wound infection following catheter removal in a PD patient was reported. We assumed that FHCS in the present case was also complicated by a delayed post-operative micro-infection after peritoneal catheter removal, rather than by PD. Thus, FHCS should be considered in PD patients with pleuritic-type RUQ abdominal pain. Biphasic CT with arterial and portal phases could help to ensure an adequate diagnosis of FHCS.
- TOOLS



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print
















