Paroxysmal nocturnal hemoglobinuria: Kidney biopsy and magnetic resonance imaging
Article information
A 39-year-old woman was referred because of oliguria and pneumonia. She had a history of unknown cause of recurrent red colored urine for 8 years despite undergoing renal biopsy in a previous hospital (Fig. 1).
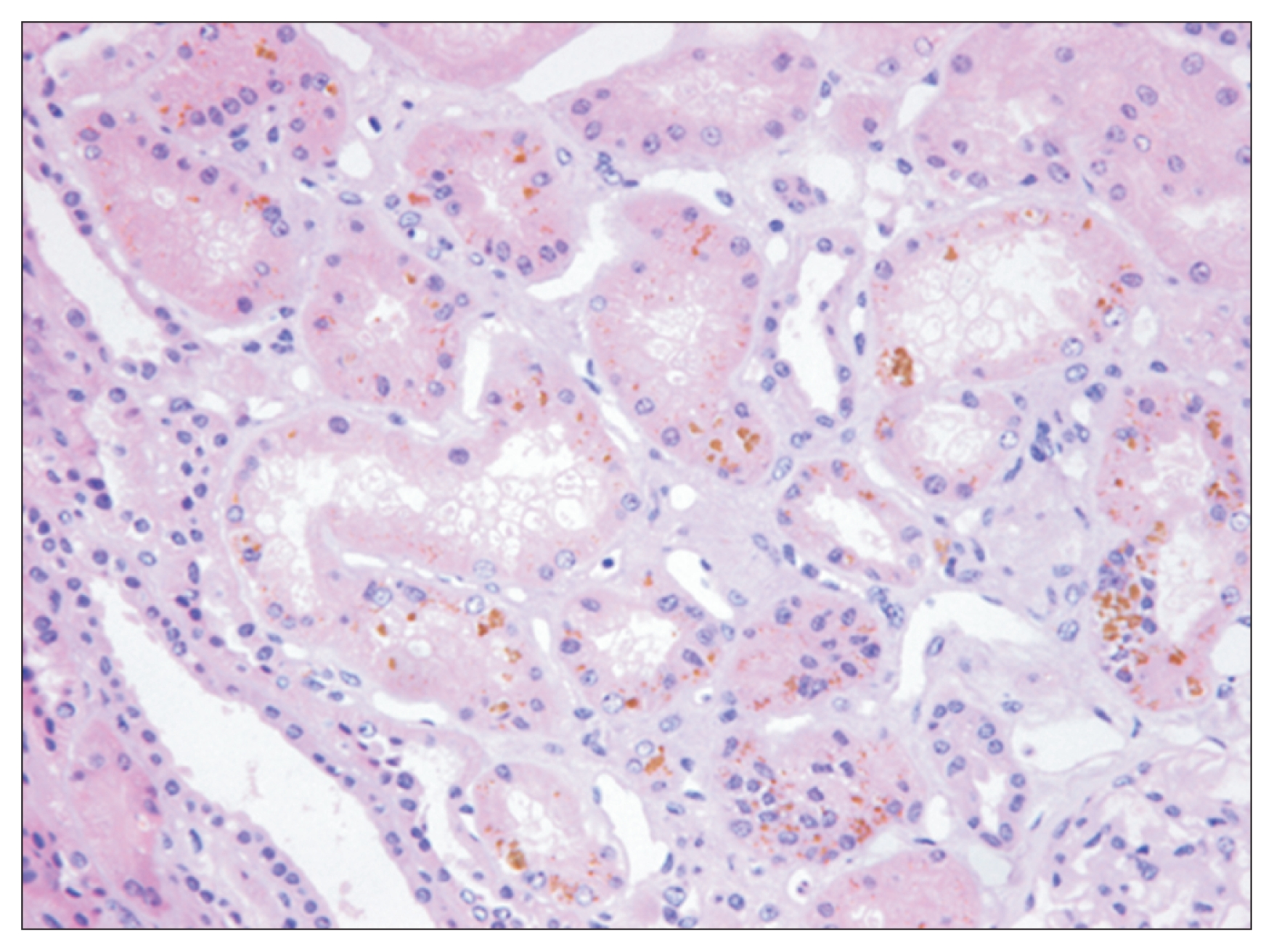
Kidney biopsy finding
Deposition of hemosiderin pigments in the proximal tubular epithelium (hematoxylineosin stain, ×400).
Initial laboratory findings showed mild anemia and moderate anisocytosis. Urinalysis showed protein (3+) and occult blood (4+). Serum creatinine had increased from 3.5 to 9.1 mg/dL in the four days after admission to our hospital. Serum immunoglobulin and complements were within normal range, and antineutrophil cytoplasmic antibody was absent. Haptoglobin level was 5 (reference range, 30–200) mg/dL, and plasma hemoglobin level was 23 (reference range, 0–5) mg/dL. Her history and laboratory findings were consistent with intravascular hemolysis. Therefore, we suspected paroxysmal nocturnal hemoglobinuria (PNH) and performed magnetic resonance imaging (MRI) of the abdomen to check for characteristic findings of PNH kidney and to rule out structural causes of acute kidney injury (AKI). MRI revealed unique findings of PNH with reversal of the renal cortico-medullary pattern in T1-weighted images (Fig. 2A) and markedly reduced signal intensity of the cortex in T2-weighted images (Fig. 2B). Flow cytometry of erythrocytes showed reduced levels of CD55 and CD59, confirming the diagnosis of PNH.

Magnetic resonance imaging
(A) The coronal T1-weighted image reveals a low cortical signal intensity in both kidneys. (B) The coronal T2-weighted image shows mild swelling of both kidneys and a low signal intensity of the renal cortex, resulting in reversed cortico-medulla differentiation.
PNH is a rare hematologic disorder caused by mutation of the PIGA gene to result in complement-induced intra-vascular hemolysis. The most consistent finding of renal biopsy in patients with PNH is hemosiderin deposition in the renal tubular cells. The characteristic MRI findings of the kidneys include reversed renal cortex-medulla differentiation on T1-weighted images and low signal intensity on both T1- and T2-weighted images. We report a case of PNH with AKI that showed typical renal histologic features and unique MRI findings simultaneously.
Notes
Conflicts of interest
All authors had no conflicts of interest to declare.