2. Middleton A, Fritz SL, Lusardi M. Walking speed: the functional vital sign.
J Aging Phys Act 2015;23:314–322.


3. Kooman JP, Kotanko P, Schols AM, Shiels PG, Stenvinkel P. Chronic kidney disease and premature ageing.
Nat Rev Nephrol 2014;10:732–742.



5. Tran J, Ayers E, Verghese J, Abramowitz MK. Gait abnormalities and the risk of falls in CKD.
Clin J Am Soc Nephrol 2019;14:983–993.



6. Cha RH, Kang SH, Han MY, An WS, Kim SH, Kim JC. Effects of AST-120 on muscle health and quality of life in chronic kidney disease patients: results of RECOVERY study.
J Cachexia Sarcopenia Muscle 2022;13:397–408.



7. Cruz-Jentoft AJ, Bahat G, Bauer J, et al. Sarcopenia: revised European consensus on definition and diagnosis.
Age Ageing 2019;48:601.



8. Chen LK, Woo J, Assantachai P, et al. Asian Working Group for Sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment.
J Am Med Dir Assoc 2020;21:300–307.


9. Abellan van Kan G, Rolland Y, Andrieu S, et al. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force.
J Nutr Health Aging 2009;13:881–889.



10. Lee YH, Lee JD, Kang DR, Hong J, Lee JM. Bioelectrical impedance analysis values as markers to predict severity in critically ill patients.
J Crit Care 2017;40:103–107.


11. Park HJ, Kim S, Yong JS, et al. Reliability and validity of the Korean version of Kidney Disease Quality of Life instrument (KDQOL-SF).
Tohoku J Exp Med 2007;211:321–329.


12. Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate.
Ann Intern Med 2009;150:604–612.



13. Mareschal J, Achamrah N, Norman K, Genton L. Clinical value of muscle mass assessment in clinical conditions associated with malnutrition.
J Clin Med 2019;8:1040.



14. Aleixo GF, Shachar SS, Nyrop KA, Muss HB, Battaglini CL, Williams GR. Bioelectrical impedance analysis for the assessment of sarcopenia in patients with cancer: a systematic review.
Oncologist 2020;25:170–182.



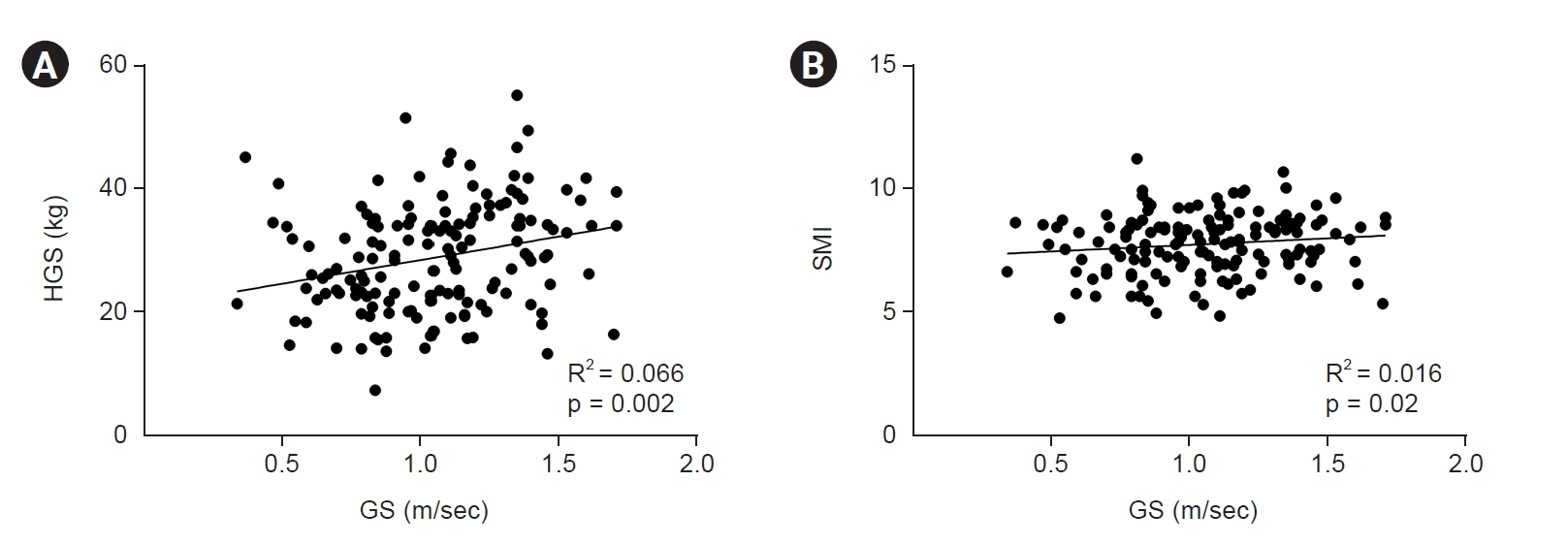
15. Li R, Xia J, Zhang XI, et al. Associations of muscle mass and strength with all-cause mortality among US older adults.
Med Sci Sports Exerc 2018;50:458–467.



16. Tsukasaki K, Matsui Y, Arai H, et al. Association of muscle strength and gait speed with cross-sectional muscle area determined by mid-thigh computed tomography: a comparison with skeletal muscle mass measured by dual-energy x-ray absorptiometry.
J Frailty Aging 2020;9:82–89.


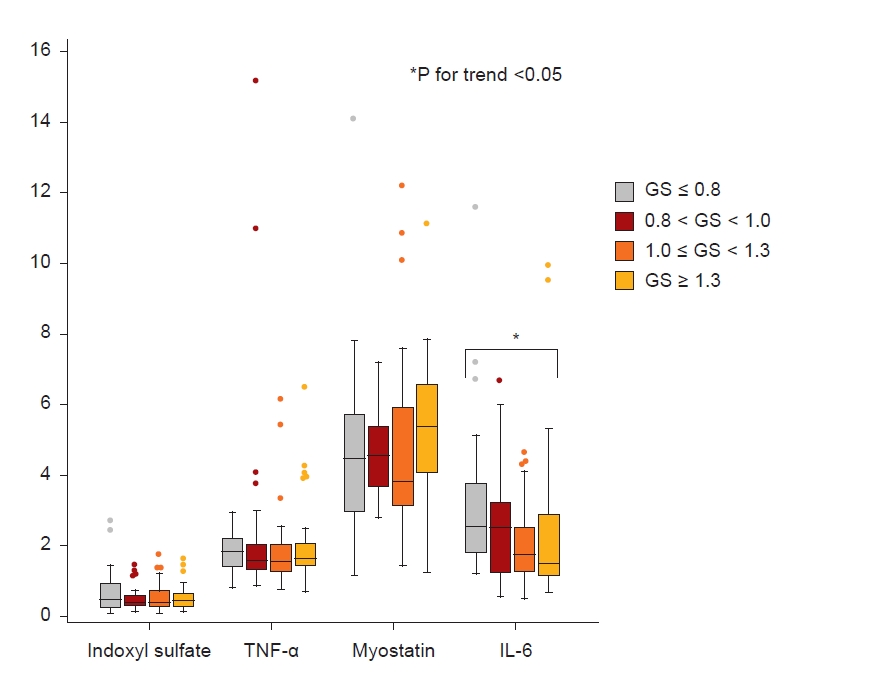
18. Kang S, Tanaka T, Narazaki M, Kishimoto T. Targeting interleukin-6 signaling in clinic.
Immunity 2019;50:1007–1023.


19. Figaro MK, Kritchevsky SB, Resnick HE, et al. Diabetes, inflammation, and functional decline in older adults: findings from the Health, Aging and Body Composition (ABC) study.
Diabetes Care 2006;29:2039–2045.

20. Wolsk E, Mygind H, Grøndahl TS, Pedersen BK, van Hall G. IL-6 selectively stimulates fat metabolism in human skeletal muscle.
Am J Physiol Endocrinol Metab 2010;299:E832–E840.


21. Verghese J, Holtzer R, Oh-Park M, Derby CA, Lipton RB, Wang C. Inflammatory markers and gait speed decline in older adults.
J Gerontol A Biol Sci Med Sci 2011;66:1083–1089.


22. Grosicki GJ, Barrett BB, Englund DA, et al. Circulating interleukin-6 is associated with skeletal muscle strength, quality, and functional adaptation with exercise training in mobility-limited older adults.
J Frailty Aging 2020;9:57–63.


23. Wang J, Leung KS, Chow SK, Cheung WH. Inflammation and age-associated skeletal muscle deterioration (sarcopaenia).
J Orthop Translat 2017;10:94–101.



26. Liaw FY, Kao TW, Fang WH, Han DS, Chi YC, Yang WS. Increased follistatin associated with decreased gait speed among old adults.
Eur J Clin Invest 2016;46:321–327.


27. White TA, LeBrasseur NK. Myostatin and sarcopenia: opportunities and challenges: a mini-review.
Gerontology 2014;60:289–293.



29. Rodrigues GG, Dellê H, Brito RB, et al. Indoxyl sulfate contributes to uremic sarcopenia by inducing apoptosis in myoblasts.
Arch Med Res 2020;51:21–29.


30. Caldiroli L, Armelloni S, Eskander A, et al. Association between the uremic toxins indoxyl-sulfate and p-cresyl-sulfate with sarcopenia and malnutrition in elderly patients with advanced chronic kidney disease.
Exp Gerontol 2021;147:111266.


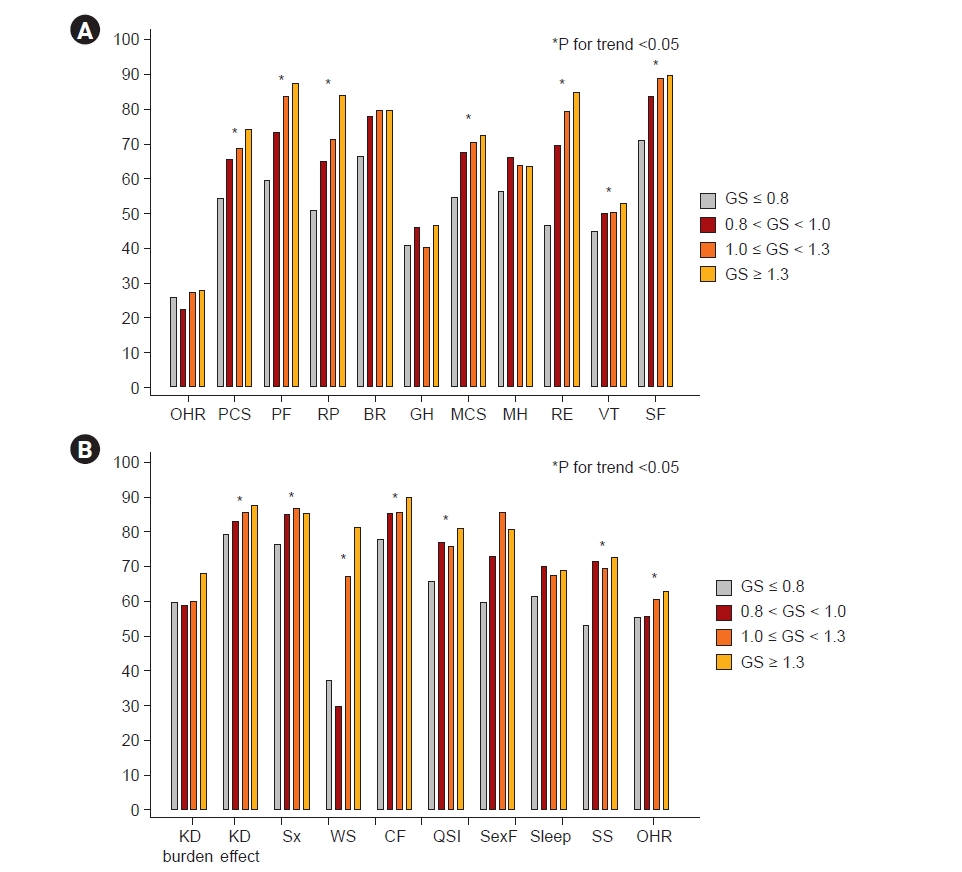
31. Marino FR, Lessard DM, Saczynski JS, et al. Gait speed and mood, cognition, and quality of life in older adults with atrial fibrillation.
J Am Heart Assoc 2019;8:e013212.



32. Wleklik M, Uchmanowicz I, Jankowska EA, et al. Multidimensional approach to frailty.
Front Psychol 2020;11:564.



33. Stringhini S, Carmeli C, Jokela M, et al. Socioeconomic status, non-communicable disease risk factors, and walking speed in older adults: multi-cohort population based study.
BMJ 2018;360:k1046.



34. Szanton SL, Seplaki CL, Thorpe RJ Jr, Allen JK, Fried LP. Socioeconomic status is associated with frailty: the Women's Health and Aging Studies.
J Epidemiol Community Health 2010;64:63–67.


36. Muscatell KA, Brosso SN, Humphreys KL. Socioeconomic status and inflammation: a meta-analysis.
Mol Psychiatry 2020;25:2189–2199.



37. Stalsberg R, Pedersen AV. Are differences in physical activity across socioeconomic groups associated with choice of physical activity variables to report?
Int J Environ Res Public Health 2018;15:922.



38. Alkerwi A, Vernier C, Sauvageot N, Crichton GE, Elias MF. Demographic and socioeconomic disparity in nutrition: application of a novel Correlated Component Regression approach.
BMJ Open 2015;5:e006814.














 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Supplement table 1
Supplement table 1 Print
Print















