| Kidney Res Clin Pract > Volume 38(1); 2019 > Article |
|
Abstract
Background
Chronic kidney disease (CKD) is associated with fluid retention, which increases total body water (TBW) and leads to changes in intracellular water (ICW) and extracellular water (ECW). This complicates accurate assessments of body composition. Analysis of bioelectrical impedance may improve the accuracy of evaluation in CKD patients and multiple machines and technologies are available. We compared body composition by bioimpedance spectroscopy (BIS) against multi-frequency bioimpedance analysis (BIA) in a multi-ethnic Asian population of stable, non-dialysis CKD patients.
Methods
We recruited 98 stable CKD patients comprising 54.1% men and 70.4% Chinese, 9.2% Malay, 13.3% Indian, and 8.2% other ethnicities. Stability was defined as no variation in serum creatinine > 20% over three months. Patients underwent BIS analyses using a Fresenius body composition monitor, while BIA analyses employed a Bodystat Quadscan 4000.
Results
Mean TBW values by BIS and BIA were 33.6 ┬▒ 7.2 L and 38.3 ┬▒ 7.4 L; mean ECW values were 15.8 ┬▒ 3.2 L and 16.9 ┬▒ 2.7 L; and mean ICW values were 17.9 ┬▒ 4.3 L and 21.0 ┬▒ 4.9 L, respectively. Mean differences for TBW were 4.6 ┬▒ 1.9 L (P < 0.001), for ECW they were 1.2 ┬▒ 0.5 L (P < 0.001), and for ICW they were 3.2 ┬▒1.8 L (P < 0.001). BIA and BIS measurements were highly correlated: TBW r = 0.970, ECW r = 0.994, and ICW r = 0.926. Compared with BIA, BIS assessments of fluid overload appeared to be more associated with biochemical and clinical indicators.
Conclusion
Although both BIA and BIS can be used for body water assessment, clinicians should be aware of biases that exist between bioimpedance techniques. The values of body water assessments in our study were higher in BIA than in BIS. Ethnicity, sex, body mass index, and estimated glomerular filtration rate were associated with these biases.
Chronic kidney disease (CKD) is associated with fluid retention, which can cause derangement of body water distribution [1]. Accurate assessment of body composition is essential for the management of CKD.
Bioelectrical impedance is a validated method to analyze body composition. It works by passing electrical currents of different frequencies through the body [2]. At low frequencies, electrical currents measure the resistance (R0) of extracellular water (ECW) [3] as they do not penetrate cell membranes. Higher-frequency currents, which do penetrate cell membranes, measure the resistance (RŌł×) of total body water (TBW) [2,4,5]. Body characteristics can be evaluated using mathematical models and empirical formulae derived from a reference population. Such characteristics include TBW, ECW, intracellular water (ICW), fat mass, lean mass, percentage body fat (% BF), and body cell mass.
Different bioimpedance technologies are employed for body composition assessments [6]. Single, dual, multifrequency, and spectroscopic methods have all been comparedŌĆöwith acceptable agreementŌĆöagainst reference methods of measuring body composition [6ŌĆō8]. Reference methods measure body spaces by radioisotope dilution [2]. However, these methods can be invasive and expensive, and cannot measure volume changes over short periods of time [2]. Multifrequency bioimpedance analysis (BIA) assesses resistance at different frequencies and factors them into empirical linear regression models to measure body composition [9]. Bioimpedance spectroscopy (BIS) uses mathematical modeling and mixture equations such as the ColeŌĆōCole and Hanai formulae to derive relationships between resistance and body fluid compartments to evaluate body composition [9]. Although both methods are commonly used, differences in accuracy and bias have been reported [2,9].
Bioimpedance techniques have been widely used for many studies involving end-stage CKD patients on dialysis [10ŌĆō12]. However, only a few studies compare the use of bioimpedance in pre-dialysis CKD patients of different ethnicities [13ŌĆō15]. Body composition analysis is essential in pre-dialysis kidney patients to optimize nutritional and fluid status [16]. Moreover, the relationship between BIA and body composition in adolescents is ethnicity-dependent and equations used for one ethnic group may not apply to another [17]. The variety of bioimpedance methods makes it important to ascertain the degree of bias between methods and instruments, and correlate these relationships to clinical findings and outcomes [18]. In this study, we compared body composition assessments in BIS against BIA in a multi-ethnic Asian population of stable, non-dialysis CKD patients.
We recruited 98 stable, non-dialysis CKD patients whose serum creatinine had not varied by > 20% over three months. The mean age of the patients was 59.9 ┬▒ 12.6 years, 70.4% were Chinese, 8.2% were Malays, 13.3% were Indians, and 8.2% were of another ethnicity. This was an approved clinical research study by the Singapore National Healthcare Group Domain Specific Review Board (DSRB) with consenting human participants (DSRB/IRB number: 2011/00325).
Anthropometry and blood samples were obtained on the day of recruitment. Serum creatinine was measured using a serum creatinase method traceable to SRM 976 on the Siemens Advia platform (Siemens, Munich, Germany). Serum prealbumin and N-terminal prohormone of brain natriuretic peptide (NT-proBNP) were assayed on the Architect platform (Abbot, Abbott Park, IL, USA) in the hospitalŌĆÖs main clinical laboratory. Blood pressures were measured using an automatic oscillometric manometer, according to clinical practice guidelines. A standardized dietary assessment using the subjective global assessment (SGA) was administered and scored on a seven-point scale. A higher score corresponds to a greater degree of malnutrition.
BIS was performed using a Fresenius body composition monitor (FBCM; Fresenius Medical Care AG & Co., Bad Homburg vor der H├Čhe, Germany) and BIA was performed on a Bodystat Quadscan 4000 (BQ4000; Bodystat Ltd., Douglas, UK). Measurements were taken in the supine position using two electrodes applied to the right hand and right leg.
Patients were analyzed by gender, ethnicity, categories of body mass index (BMI), and estimated glomerular filtration rate (eGFR). Ethnicity was divided into Chinese and non-Chinese Asian to reflect the multi-ethnic society of Singapore, which is 75% Chinese. BMI categories were < 25.0 kg/m2, 25.0 to 30.0 kg/m2, and > 30.0 kg/m2. Glomerular filtration rates were estimated using the CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) equation. Comparisons were made by eGFR categories < 30, 30 to 60, and > 60 mL/min/1.73 m2. Standard t test, PearsonŌĆÖs correlation, and chi-square statistical tests were applied where appropriate. To assess bioimpedance measures with clinical and biochemical outcomes, we used correlation and linear regression for continuous variables; and logistic regression for discrete variables. To assess the clinical associations of bioimpedance measures of volume, we evaluated TBW, ECW, and ECW/ICW against systolic blood pressure (SBP), diastolic blood pressure (DBP), and plasma NT-proBNP. To assess the clinical correlations of bioimpedance measures of body composition, we evaluated lean mass against serum prealbumin, mid-arm muscle circumference (MAMC), and the SGA score; and fat mass against waist circumference, skin-fold thickness, and the waist-to-hip ratio. Variables with non-normal distribution were natural log-transformed prior to analysis. A P value of < 0.05 was considered significant. Analyses were performed on statistical software of JMP (Cary, NC, USA).
The characteristics of the 98 patients are shown in Table 1.
Overall body water assessments using BIA produced higher volumes than BIS (4.6 L, P < 0.001) (Table 2). The largest differences were in men (5.4 L, P < 0.001). Overall, ECW using BIA produced higher volumes than did BIS (1.2 L, P < 0.001). The largest difference was in women (1.6 L, P < 0.001). Overall, ICW using BIA gave higher volumes than did BIS (3.2 L, P < 0.001). The largest difference was in patients with a BMI > 30 kg/m2 (4.2 L, P < 0.001). Overall, an ECW/ICW ratio using BIS produced higher values than did BIA (0.10, P < 0.001). The largest difference was in patients with a BMI > 30 kg/m2 (0.13, P < 0.001).
Within eGFR categories, BIA produced higher values than did BIS for TBW assessments. The largest difference was in patients with an eGFR < 30 mL/min/1.73 m2 (4.9 L, r = 0.968, P < 0.001). The least difference was in patients with an eGFR > 60 mL/min/1.73 m2 (4.0 L, r = 0.976, P < 0.001). For ECW assessments, the largest difference was in patients with an eGFR < 30 mL/min/1.73 m2 (1.3 L, r = 0.989, P < 0.001). The least difference was in patients with an eGFR of 30 to 60 mL/min/1.73 m2 (1.1 L, r = 0.996, P < 0.001). For ICW assessments, the largest difference was in patients with an eGFR of 30 to 60 mL/min/1.73 m2 (3.5 L, r = 0.926, P < 0.001). The least difference was in patients with an eGFR > 60 mL/min/1.73 m2 (2.6 L, r = 0.925, P < 0.001). For ECW/ICW ratios, the largest difference was in patients with an eGFR of 30 to 60 mL/min/1.73 m2 (0.11, r = 0.590, P < 0.001). The least difference was in patients with an eGFR > 60 mL/min/1.73 m2 (0.09, r = 0.421, P < 0.001).
Within BMI categories, BIA gave higher values than did BIS for TBW assessments. The largest difference was in patients with a BMI of 25.0 to 30.0 kg/m2 (5.2 L, r = 0.968, P < 0.001). The least difference was in patients with a BMI < 25 kg/m2 (4.0 L, r = 0.956, P < 0.001). For ECW assessments, the largest difference was in patients with a BMI < 25 kg/m2 (1.3, r = 0.996, P < 0.001). The least difference was in patients with a BMI > 30 kg/m2 (1.1 L, r = 0.996, P < 0.001). For ICW assessments, the largest difference was in patients with a BMI > 30 kg/m2 (4.2 L, r = 0.950, P < 0.001). The least difference was in patients with a BMI < 25 kg/m2 (2.1 L, r = 0.913, P < 0.001). For ECW/ICW ratios, the largest difference was in patients with a BMI > 30 kg/m2 (0.13, r = 0.639, P < 0.001). The least difference was in patients with a BMI < 25 kg/m2 (0.07, r = 0.493, P < 0.001).
Between Chinese and non-Chinese, BIA gave higher values than did BIS for TBW assessments. The larger difference was in Chinese (4.8 L, r = 0.973, P < 0.001). For ECW assessments, the larger difference was in non-Chinese (1.2 L, r = 0.995, P < 0.001) (Table 2). For ICW assessments, the larger difference was in Chinese (3.2 L, r = 0.934, P < 0.001). For ECW/ICW ratios, the larger difference was in non-Chinese (0.10, r = 0.451, P < 0.001).
Between men and women, BIA produced higher values than did BIS for TBW assessments. The larger difference was in men (5.4 L, r = 0.935, P < 0.001). For ECW assessments, the larger difference was in women (1.6 L, r = 0.993, P < 0.001). For ICW assessments, the larger difference was in men (3.9 L, r = 0.857, P < 0.001). For ECW/ICW ratios, the larger difference was in men (0.11, r = 0.793, P < 0.001).
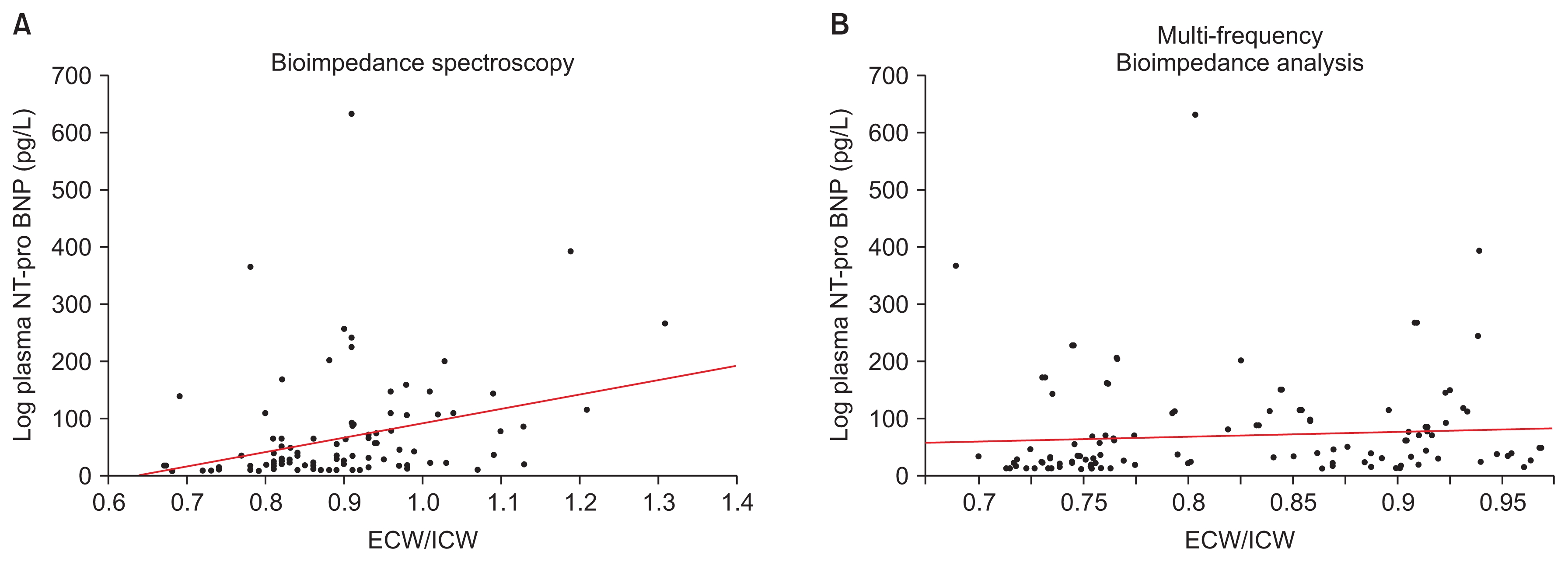
Log plasma NT-proBNP was associated with the ratio of ECW/ICW obtained by BIS (log plasma NT-proBNP = ŌłÆ153.88 + 248.60 ├Ś ECW/ICW, P = 0.003) (Fig. 1). TBW and ECW measured by BIS and BIA, and ECW/ICW obtained by BIA were not associated with log plasma NT-proBNP. SBP was associated with the ratio of ECW/ICW measured by BIS (SBP = 89.54 + 53.39 ├Ś ECW/ICW, P < 0.001) (Fig. 2). DBP was associated with log ECW/ICW evaluated by BIA (DBP = 102.52 ŌłÆ 35.28 ├Ś ECW/ICW, P = 0.004). TBW and ECW measured by BIS or BIA were not associated with SBP or DBP.
Overall lean mass assessments using BIA gave higher values than did BIS (11.1 kg, P < 0.001) (Table 3). The largest difference was in patients with a BMI > 30 kg/m2 (15.9 kg, P < 0.001). Overall fat mass assessments using BIS gave higher values than did BIA (2.1 kg, P < 0.001) (Table 3). The largest difference was in men (3.6 kg, P < 0.001).
Overall, % BF assessments using BIS produced higher values than did BIA (2.6%, P < 0.001) (Table 3). The largest difference was in men (4.4%, P < 0.001). Overall, body cell mass assessments using BIA gave higher values than BIS (9.9, P < 0.001) (Table 3). The largest difference was in patients with a BMI > 30 kg/m2 (12.8, P < 0.001). BIA assessments were highly correlated with BIS.
Within eGFR categories, BIA produced higher values for lean mass and body cell mass assessments. BIS produced higher values for fat mass and % BF assessments. For lean fat assessments, the largest difference was in patients with an eGFR < 30 mL/min/1.73 m2 (12.2 kg, r = 0.906, P < 0.001) (Table 3). The least difference was in patients with an eGFR > 60 mL/min/1.73 m2 (11.4kg, r = 0.871, P < 0.001). For fat mass assessments, the largest difference was in patients with an eGFR of 30 to 60 (3.4 kg, r = 0.884, P < 0.001) (Table 3). The least difference was in patients with an eGFR < 30 mL/min/1.73 m2 (2.5 kg, r = 0.954, P < 0.001). For % BF assessments, the largest difference was in patients with an eGFR > 60 mL/min/1.73 m2 (4.4%, r = 0.895, P < 0.001) (Table 3). The least difference was in patients with an eGFR < 30 mL/min/1.73 m2 (3.3%, r = 0.948, P < 0.001). For body cell mass, the largest difference was in patients with an eGFR < 30 mL/min/1.73 m2 (10.6 kg, r = 0.891, P < 0.001) (Table 3). The least difference was in patients with an eGFR > 60 mL/min/1.73 m2 (8.7 kg, r = 0.828, P < 0.001).
Within BMI categories, BIA produced higher values for lean mass and body cell mass assessments. BIS gave higher values for fat mass and % BF assessments. For lean mass assessments, the largest difference was in patients with a BMI > 30 kg/m2 (15.9 kg, r = 0.938, P < 0.001) (Table 3). The least difference was in patients with a BMI < 25 kg/m2 (7.9 kg, r = 0.902, P < 0.001). For fat mass assessments, the largest difference was in patients with a BMI > 30 kg/m2 (3.9 kg, r = 0.806, P < 0.001) (Table 3). The least difference was in patients with a BMI < 25 kg/m2 (2.1 kg, r = 0.811, P < 0.001). For % BF assessments, the largest difference was in patients with a BMI of 25.0 to 30.0 kg/m2 (4.8%, r = 0.890, P < 0.001) (Table 3). The least difference was in patients with a BMI < 25 kg/m2 (3.4%, r = 0.868, P < 0.001). For body cell mass assessments, the largest difference was in patients with a BMI > 30 kg/m2 (12.8 kg, r = 0.911, P < 0.001) (Table 3). The least difference was in patients with a BMI < 25 kg/m2 (7.4 kg, r = 0.873, P < 0.001).
For both Chinese and non-Chinese, BIA resulted in higher values for lean mass and body cell mass assessments. Conversely, BIS resulted in higher values for fat mass and % BF assessments. For lean mass assessments, the larger difference was in Chinese (11.7 kg, r = 0.883, P < 0.001) (Table 3). For fat mass assessments, the larger difference was in Chinese (3.2 kg, r = 0.892, P < 0.001) (Table 3). For % BF assessments, the larger difference was in Chinese (4.3%, r = 0.855, P < 0.001) (Table 3). For body cell mass assessments, the larger difference was in non-Chinese (9.8 kg, r = 0.873, P < 0.001) (Table 3).
Between men and women, BIA resulted in higher values for lean mass and body cell mass assessments. BIS resulted in higher values for fat mass and %BF assessments. Men had larger differences for lean mass assessments (12.9 kg, r = 0.702, P < 0.001) (Table 3), fat mass assessments (4.2 kg, r = 0.921, P < 0.001) (Table 3), % BF assessments (5.4 kg, r = 0.921, P < 0.001) (Table 3) and body cell mass assessments (10.4 kg, r = 0.686, P < 0.001) (Table 3).
Waist circumference was associated with fat mass assessments in both BIS (waist circumference = 69.97 + 0.97 ├Ś fat mass, P < 0.001) and BIA (waist circumference = 73.81 + 0.89 ├Ś fat mass, P < 0.001). Skin-fold thickness was also associated with fat mass assessments in both BIS (skin-fold thickness = 1.58 + 0.07 ├Ś fat mass, P < 0.001) and BIA (skin-fold thickness = 1.79 + 0.06 ├Ś fat mass, P < 0.001). Fat mass assessments were not associated with waist-to-hip ratio. Serum prealbumin was associated with lean mass measurement in BIS (prealbumin = 25.50 + 0.13 ├Ś lean mass, P = 0.020) but not with lean mass evaluated in BIA. SGA scores were also only associated with lean mass by BIS (ŌłÆlog likelihood 2.667, chi-square = 5.334, P = 0.0209). Conversely, MAMC was associated with lean mass in both BIS (MAMC = 11.700 + 0.034 ├Ś lean mass, P = 0.0049) and BIA (MAMC = 11.451 + 0.0305 ├Ś lean mass, P = 0.0036).
Our results showed clinically significant biases in body composition assessments in BIA and BIS using the FBCM and the BQ400. On average, BIA recorded higher readings for TBW, ECW, ICW, and lean mass but lower values for fat mass and % BF. Subgroup analyses of the study population were carried out to delineate the biases based on specific patient profiles. The biases varied with ethnicity, sex, BMI, and eGFR.
Body composition assessment is required in pre-dialysis patients to assess nutrition and change in fluid status. In an earlier study, we showed that pre-dialysis CKD patients have poorly controlled hypertension despite being treated in an academic medical center [19]. Furthermore, National Kidney Foundation clinical practice guidelines recommend nutritional assessment in CKD and end-stage kidney disease to maintain adequate muscle mass [16]. Bioimpedance techniques allow clinicians to accurately assess a patientŌĆÖs body composition. Patients who have a high ECW and are hypertensive can be treated with sodium restriction and anti-hypertensives [20]. Moreover, patients with declining muscle mass can be prescribed protein supplements and exercise therapies [16,20].
Differences in body water and lean mass assessments were greatest in patients with an eGFR < 30 mL/min/1.73 m2. In CKD patients, we are usually interested in the distribution of body water as a higher ratio of ECW/ICW suggests fluid overload [21]. Objective assessments of lean fat mass are also important. In earlier stages, higher adiposity may be associated with metabolic syndrome, and thus detrimental to kidney function. In advanced CKD, adequate lean mass and body fat may be protective against infections and mortality during the transition to end-stage kidney disease and the initiation of dialysis [13,14,22ŌĆō24].
The various body water assessments differed in our study. For TBW, the largest differences recorded were in men and in patients with an eGFR < 30 mL/min/1.73 m2, a BMI between 25.0 to 30.0 kg/m2, or Chinese ethnicity. In ECW, the largest differences recorded were in women and patients with an eGFR < 30 mL/min/1.73 m2, a BMI < 25 kg/m2, or non-Chinese ethnicity. These factors resulted in higher BIS-determined ECW/ICW ratios, especially in patients with an eGFR of 30 to 60 mL/min/1.73 m2, a BMI > 30 kg/m2, or non-Chinese ethnicity, and in men. ECW had the highest correlation (r = 0.994) followed by TBW (r = 0.970), ICW, (r = 0.926), and ECW/ICW ratio (r = 0.499). These findings suggest that these biases must be borne in mind when using BQ4000 BIA analyses of body water distribution to manage fluid overload, and that the resulting assessments are not equivalent to those of FBCM BIS. Regardless of the absolute numerical values, correlation with outcomes during clinical intervention is required for practical application.
The FBCM BIS ECW/ICW ratios appear to be more valid in their correlation with elevated SBP and plasma NT-proBNP, both of which are indicative of fluid overload and expanded intravascular volume [25ŌĆō27]. While BIA ECW/ICW ratios were correlated with DBP and not SBP, the limitations of DBP as a reliable hypertensive factor in clinical outcomes have been reported extensively [28ŌĆō30]. SBP rises with age, while DBP tends to fall in patients > 50 years old [28]. Furthermore, reduction of SBP has been shown to be a better predictor of cardiovascular events and thus has become the primary target of anti-hypertensive therapy [30].
In assessing lean mass, the largest differences recorded were in men, non-Chinese, or those with an eGFR < 30 mL/min/1.73 m2 or BMI > 30 kg/m2. The highest correlation was in fat mass (r = 0.982), followed by lean mass (r = 0.981), body cell mass (r = 0.941), and % BF (r = 0.931). The reported biases are likely to be inherent in the methods used in both instruments. In developing the FBCM BIS, the derivation population included CKD patients, whereas BQ4000 BIA may not have adequate representation. Because no derivation equations within these machines were made using reference methods in Asians, no adjustment factors were available; the equations within the machines are proprietary. Other factors, including the number of frequencies employed and the mathematical models assumed in estimating body compartments, may affect the estimates. The FBCM BIS uses 50 frequencies that range from 5 to 1,000 kHz. The BQ4000 BIA assesses body composition using only four impedance values: 5, 50, 100, and 200 kHz.
Bioimpedance methods have been validated against reference standards [15,18]. In a population of 36 healthy males, ECW and TBW measured with BIA with reference radioisotope dilution methods had a high correlation of r = 0.930 and r = 0.947, respectively [31]. However, overestimation of TBW and ECW using BIA in obese people has also been reported [32]. These results are similar to our study of stable CKD patients. Furthermore, our results showed that BIS and BIA were associated with skin-fold thickness in pre-dialysis CKD patients although skin-fold thickness has been reported to be more reliable than BIS for fat assessment [33]. BIA is widely used in many centers [15]. Also, selection of a specific bioimpedance method has yet to become universal for CKD patients. While our study did not prove which method was more accurate, it emphasized the importance of knowing the relative bias of measurements obtained in patients with pre-dialysis CKD. Furthermore, the information derived from BIS and BIA is not directly interchangeable. It is important for clinicians to safely and correctly interpret and apply the measurements obtained from various instruments in their clinical practices. Regardless of the bioimpedance method used, clinical correlation is essential.
This study has a number of limitations. First, the majority of patients had a BMI > 25 kg/m2, which may have skewed the results. Second, body composition (muscle and fat) may have been influenced by ethnicity as we had fewer non-Chinese patients. Third, our study did not compare bioimpedance measurements to values obtained by reference methods for assessing body water distribution, body muscle, and fat composition. However, the aim of this study was to determine the degree of biases within both methods of bioimpedance. Fourth, the BIS machine had been validated for managing fluid volume in dialysis patients. Most of the patients in this study were stable, non-dialysis CKD patients who underwent a cross-sectional assessment of body composition with no clinical intervention to assess the veracity of the bioimpedance measures longitudinally.
In conclusion, this study showed that biases exist when using either the FBCM BIS or the BQ4000 BIA. Ethnicity, sex, BMI, and eGFR contributed to the differences. FBCM BIS volume assessments of fluid overload appear to be more strongly associated with biochemical and clinical indicators.
Acknowledgments
We acknowledge other members of the Division of Nephrology who contributed patients toward this study: Professor Vathsala, Dr Srinivas Subramanian, Dr Her-sharan Sran Kaur, Dr Behram Ali Khan, Dr Muhammad Javaid, and Dr Martin Lee. Other key contributors were Dr Sharon Saw and Mr Qi Chun Toh.
Figure┬Ā1
Bivariate fit of log plasma B-type natriuretic peptide (plasma NT-pro BNP)
(A) Bivariate fit of log plasma NT-pro BNP by BIS extracellular water/intracellular water (ECW/ICW) (log plasma NT-proBNP = ŌłÆ153.88 + 248.60 ├Ś ECW/ICW, P = 0.003). (B) Bivariate fit of log plasma NT-proBNP by BIA ECW/ICW (log plasma NT-proBNP = 1.019 + 83.041 ├Ś ECW/ICW, P = 0.480).
BIA, bioimpedance analysis; BIS, bioimpedance spectroscopy.
Figure┬Ā2
Bivariate fit of systolic blood pressure (SBP)
(A) Bivariate fit of SBP by BIS extracellular water/intracellular water (ECW/ICW) (SBP = 89.54 + 53.39 ├Ś ECW/ICW, P < 0.001). (B) Bivariate fit of SBP by BIA ECW/ICW (SBP = 127.21 + 12.49 ├Ś ECW/ICW, P = 0.560).
BIA, bioimpedance analysis; BIS, bioimpedance spectroscopy.

Table┬Ā1
Patient demographics and characteristics
Table┬Ā2
Body water assessments
Table┬Ā3
Body composition assessments
References
1. Hassan MO, Duarte R, Dix-Peek T, et al. Volume overload and its risk factors in South African chronic kidney disease patients: an appraisal of bioimpedance spectroscopy and inferior vena cava measurements. Clin Nephrol 2016;86:27ŌĆō34.

2. Hannan WJ, Cowen SJ, Plester CE, Fearon KC, deBeau A. Comparison of bio-impedance spectroscopy and multi-frequency bio-impedance analysis for the assessment of extracellular and total body water in surgical patients. Clin Sci (Lond) 1995;89:651ŌĆō658.


3. Thomas BJ, Cornish BH, Ward LC. Bioelectrical impedance analysis for measurement of body fluid volumes: a review. J Clin Eng 1992;17:505ŌĆō510.

4. Abbas SR, Liu L, Sipahioglu MH, et al. Comparison of bio-impedance techniques to detect changes in fluid status in hemodialysis patients. Blood Purif 2014;37:48ŌĆō56.


5. Matthie JR. Bioimpedance measurements of human body composition: critical analysis and outlook. Expert Rev Med Devices 2008;5:239ŌĆō261.


6. El-Kateb S, Davenport A. Changes in hydration following haemodialysis estimated with bioimpedance spectroscopy. Nephrology 2016;21:410ŌĆō415.


7. Shaikh MG, Crabtree NJ, Shaw NJ, Kirk JM. Body fat estimation using bioelectrical impedance. Horm Res 2007;68:8ŌĆō10.

8. Silva AM, Heymsfield SB, Gallagher D, et al. Evaluation of between-methods agreement of extracellular water measurements in adults and children. Am J Clin Nutr 2008;88:315ŌĆō323.



9. Kyle UG, Bosaeus I, De Lorenzo AD, et al. Composition of the ESPEN Working Group. Bioelectrical impedance analysis--part I: review of principles and methods. Clin Nutr 2004;23:1226ŌĆō1243.


10. Kushner RF, de Vries PM, Gudivaka R. Use of bioelectrical impedance analysis measurements in the clinical management of patients undergoing dialysis. Am J Clin Nutr 1996;64(3 Suppl):503SŌĆō509S.


11. Castellano S, Palomares I, Moissl U, et al. Appropriate assessment of body composition to identify haemodialysis patients at risk. Nefrologia 2016;36:268ŌĆō274.


12. Hung SC, Kuo KL, Peng CH, Wu CH, Wang YC, Tarng DC. Association of fluid retention with anemia and clinical outcomes among patients with chronic kidney disease. J Am Heart Assoc 2015;4:e001480



13. Bellizzi V, Scalfi L, Terracciano V, et al. Early changes in bio-electrical estimates of body composition in chronic kidney disease. J Am Soc Nephrol 2006;17:1481ŌĆō1487.


14. Cupisti A, DŌĆÖAlessandro C, Morelli E, et al. Nutritional status and dietary manipulation in predialysis chronic renal failure patients. J Ren Nutr 2004;14:127ŌĆō133.


15. Caravaca F, Mart├Łnez del Viejo C, Villa J, Mart├Łnez Gallardo R, Ferreira F. Hydration status assessment by multi-frequency bioimpedance in patients with advanced chronic kidney disease. Nefrologia 2011;31:537ŌĆō544.

16. Kopple JD. National kidney foundation K/DOQI clinical practice guidelines for nutrition in chronic renal failure. Am J Kidney Dis 2001;37(1 Suppl 2):S66ŌĆōS70.


17. Sluyter JD, Schaaf D, Scragg RK, Plank LD. Prediction of fatness by standing 8-electrode bioimpedance: a multiethnic adolescent population. Obesity (Silver Spring) 2010;18:183ŌĆō189.


18. Jackson AA, Johnson M, Durkin K, Wootton S. Body composition assessment in nutrition research: value of BIA technology. Eur J Clin Nutr 2013;67(Suppl 1):S71ŌĆōS78.


19. Teo BW, Chua HR, Wong WK, et al. Blood pressure and antihypertensive medication profile in a multiethnic Asian population of stable chronic kidney disease patients. Singapore Med J 2016;57:267ŌĆō273.



20. National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 2002;39(2 Suppl 1):S1ŌĆōS266.

21. Abbas SR, Zhu F, Levin NW. Bioimpedance can solve problems of fluid overload. J Ren Nutr 2015;25:234ŌĆō237.


23. Nazar CM, Bojerenu MM, Safdar M, Ahmed A, Akhtar MH, Kindratt TB. Efficacy of dietary interventions in end-stage renal disease patients; a systematic review. J Nephropharmacol 2015;5:28ŌĆō40.


25. Booth J, Pinney J, Davenport A. N-terminal proBNP--marker of cardiac dysfunction, fluid overload, or malnutrition in hemodialysis patients? Clin J Am Soc Nephrol 2010;5:1036ŌĆō1040.



26. Crepaldi C, Lamas EI, Martino FK, et al. Bioimpedance and brain natriuretic peptide in peritoneal dialysis patients. Contrib Nephrol 2012;178:174ŌĆō181.


27. Nongnuch A, Panorchan K, Davenport A. Predialysis NT-proBNP predicts magnitude of extracellular volume overload in haemodialysis patients. Am J Nephrol 2014;40:251ŌĆō257.


29. Powell TM, Glynn RJ, Buring JE, Creager MA, Ridker PM, Pradhan AD. The relative importance of systolic versus diastolic blood pressure control and incident symptomatic peripheral artery disease in women. Vasc Med 2011;16:239ŌĆō246.



30. Strandberg TE, Pitkala K. What is the most important component of blood pressure: systolic, diastolic or pulse pressure? Curr Opin Nephrol Hypertens 2003;12:293ŌĆō297.


31. Segal KR, Burastero S, Chun A, Coronel P, Pierson RN Jr, Wang J. Estimation of extracellular and total body water by multiple-frequency bioelectrical-impedance measurement. Am J Clin Nutr 1991;54:26ŌĆō29.





 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print
















