Introduction
The number of end-stage renal disease (ESRD) patients undergoing maintenance dialysis therapy has increased very rapidly in recent decades because of the increase of elderly population and diabetic patients all over the world. Maintenance dialysis for ESRD is one of typical therapies for long-term vital organ replacement, which is considered as the most cost-consuming treatment in current medical practice. For adequate supply of dialysis facilities and proper management of dialysis therapy itself, nationwide statistical data and analysis are essential.
In Korea, the first nationwide survey on dialysis was performed by the late Professor Byung-Suk Min in 1980 and was published in the first issue of Korean Journal of Nephrology, which was previously the official journal of the Korean Society of Nephrology (KSN) [1]. The KSN launched a nationwide official survey program about dialysis therapy in 1985. Nowadays, the accumulated data for 30 years by this “Insan Prof. Min Memorial ESRD Registry” program have been providing essential information for dialysis clinical practice, academic nephrology research, and health management policy [2,3].
We reviewed 30 years of data to identify important changes and implications for the future improvement of dialysis therapy in Korea.
Development of the registry process
From 1985 to 1994, a printed questionnaire was posted to every dialysis center in Korea, mainly university hospitals, and replied mails were also posted back to the KSN office. As personal computers were used in most hospitals, the KSN developed an electronic questionnaire about dialysis in 1995 and posted it on a diskette to every dialysis center. The replies were also posted on diskettes or transmitted via electronic file transfer through a dial-up modem. An Internet questionnaire was developed in 2001, which was completely revised in 2013 for updates of dialysis therapy and data security. Currently, the Internet questionnaire includes dialysis center information, patient personal medical information, vascular access, dialysis adequacy performance data, medications including erythropoietin (EPO) and phosphate binders, rehabilitation status, and laboratory data. The program also has a graphic evaluation function of dialysis adequacy: single-pool Kt/V, normalized protein catabolic rate, and a peritoneal equilibrium test. The data were collected on the KSN Web page throughout the year (Table 1). Every KSN member can access the dialysis adequacy data of their own dialysis center anytime, which could be of some help for dialysis prescriptions. The average KSN ESRD registry response rate of the past 3 years was about 70%. The annual survey results have been reported at the autumn meeting of the KSN and on the KSN Web page, and currently reported at the spring KSN meeting since 2014.
Dialysis data from the KSN ESRD registry
Prevalence and incidence of ESRD
At the end of 2014, the number of ESRD patients in Korea was reported as 80,674, in which 57,256 were hemodialysis (HD) patients, 7,423 were peritoneal dialysis (PD) patients, and 15,995 were kidney transplantation (KT) patients. The patient per million population was 1,115 HD, 145 PD, 311 KT, and overall 1,572 [4]. In addition, the proportions of HD, PD, and KT in renal replacement modalities were 71%, 9%, and 20%, respectively, at the end of 2014 (Fig. 1A).
The Korean prevalence rate of ESRD patients was about 70% of the United States and about 50% of Japan according to the international comparisons in the annual data report of United States Renal Data System (USRDS) [5,6]. The increase of the number of HD patients was still high at 9% per year, but there was nearly no increase in the number of PD patients in recent years.
The number of new patients with dialysis initiation in 2014 was estimated to be 11,461 (10,594 HD, 867 PD, overall 213 patients per million population).
Underlying causes of ESRD
The most common underlying cause of ESRD is diabetic nephropathy, which was 48% in new ESRD patients in 2014. Other common causes were hypertensive nephrosclerosis (21.2%) and chronic glomerulonephritis (8.2%). The proportion of diabetic patients in Korea was the highest in the world, except for a couple of city states according to international comparisons in the annual data report of USRDS. The diabetic proportion rapidly increased from 1990 to 2000 but slowly increased from 2000 to 2014 in Korea (Fig. 1B).
Dialysis centers and dialysis machines
The number of dialysis centers in Korea was 763, in which the non-KSN member centers (approximately 40 centers) were excluded. The number of HD machines was estimated at 21,000 at the end of 2014. The average number of machines per center was about 28, and the average number of HD patients per machine was 2.7. About 47% of HD patients were under maintenance dialysis therapy at private clinics, about 36% patients were at a general hospital, and about 17% of patients were at a university hospital. The proportion of general hospitals increased because of the increase of dialysis centers for elderly patients in nursing hospitals.
Dialysis patient characteristics
Sex ratio
The sex ratio (male vs. female) was 58%:42% in HD patients and 56%:44% in PD patients. The number of male patients was much higher than the number of female patients compared with the general population. These ratios had no interval change during 20 years and were quite similar to those of the United States.
ABO blood type
The ratio of ABO blood type (A:B:AB:O) was 35%:27%:11%:27%, which was the same as the general population.
Hepatitis B and C
Hepatitis B antigen positivity was 6% and hepatitis C antibody positivity was 4% in HD patients in 2014. The percentages in PD patients were 6% and 3%, respectively.
Medical insurance status
About 76% of dialysis patients were covered by national health insurance and 20% were under medical aid programs in Korea at the end of 2014.
Age
The average age of overall dialysis patients was 60.3±14.1 years, which had steadily increased from 55.2 years in 2005. The average age of HD patients was 61.1±13.8 years and 55.4 ±14.5 years in PD patients. The percentage of elderly patients (over 65 years) was 40.7% in 2014, which had increased from 28% in 2005. The average age of diabetic dialysis patients was 62.7±12.2 years, hypertensive nephrosclerosis patients was 61.5±13.9 years, and chronic glomerulonephritis patients was 54.5±15.0 years in 2014 (Fig. 1C).
Duration of dialysis maintenance
About 21% of HD patients were under dialysis therapy for more than 10 years, and 27% of HD patients were under 5–10 years, and 11% were under less than 1 year of dialysis therapy. Among PD patients, only 15% were under dialysis for more than 10 years. In addition, about 11% of diabetic HD patients were under dialysis for more than 10 years, but 29% of nondiabetic HD patients were under dialysis for more than 10 years. These data suggested that the survival of HD patients and nondiabetic patients is longer than that of PD patients and diabetic patients (Fig. 1D).
Body mass index
The average of body mass index (the body weight in kilogram divided by square of the body height in meters) of HD patients was 22.2±4.1 kg/m2 and that of PD patients was 24.2±5.1 kg/m2 in 2014. These were also steadily increased from 21.4 kg/m2 and 23.2 kg/m2 in 2005.
Blood pressure
The mean arterial pressure of HD patients was 100.0±12.2 mmHg and that of PD patients was 97.9±13.7 mmHg in 2014. These mean arterial pressures decreased from 104.9 mmHg and 100.4 mmHg in 2005. The mean pulse pressure of HD patients was 65.2±17.3 mmHg, which was much higher than that of PD patients, 53.7±13.6 mmHg (Figs. 1 E and 1F).
Dialysis therapy characteristics
Frequency of HD and hemodiafiltration (HDF). About 91% of HD patients were on a three times/wk schedule and only 7% of patients were on a twice/wk schedule. The percentage had minimally changed from 2005. HDF therapy was still not popular and was provided to only 15% of HD patients.
Dialyzer and dialysate
The surface area of dialyzer had been slowly increasing, but only 50% of HD patients were under dialysis with a less than 1.5 m2 dialyzer, and a 1.5 m2 to 2.0 m2 dialyzer was used for 44% of HD patients. The bicarbonate dialysate was used for about 97% of HD patients, dialysate with glucose was used for 65% of HD patients, and low calcium dialysate was used for 6% of HD patients.
Vascular access
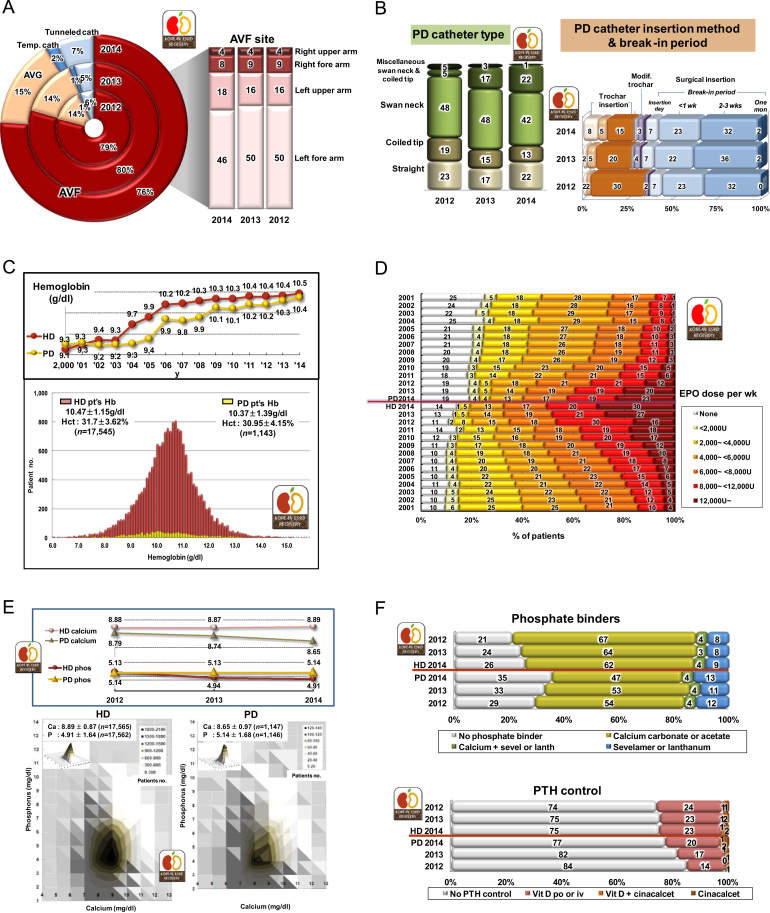
The autologous arteriovenous fistula was used in 76% of HD patients, arteriovenous graft shunt was used in 15%, and subcutaneous tunneled catheter was used in 7% of HD patients. About 46% of HD patients had the arteriovenous fistula on the left forearm and 18% had fistula on the left upper arm in 2014 (Fig. 2A).
PD catheters
About 42% of PD patients had swan neck PD catheters and 22% had swan neck with coiled tip PD catheters in 2014. The PD catheter was inserted by surgical method in 64% and by trocar method in 28% of newly started PD patients in 2014. The break-in period of the PD catheter was mostly 2–3 weeks (32%) (Fig. 2B).
PD type and doses
The automated PD program was applied to about 26% of PD patients in 2014. About 52% of PD patients had used 8–10 L/d of dialysate.
Anemia and EPO therapy
The mean hemoglobin level of HD patients was 10.47±1.15 g/dL and that of PD patients was 10.37±1.39 g/dL in 2014. More than 12,000 units/wk of EPO was injected to 30% of HD patients, but only 14% of HD patients had not used EPO. In PD patients, only 23% of patients had used more than 12,000 units/wk of EPO and 19% of patients had no EPO (Figs. 2C and 2D). Darbepoetin (Nesp®) and methoxy polyethylene glycol-epoetin beta (Mircera®) were calculated with conversion factor of EPO.
Calcium and phosphorus control
The mean calcium level of HD patients was 8.89±0.87 mg/dL and that of PD patients was 8.65±0.97 mg/dL in 2014. The mean phosphorus level of HD patients was 4.91±1.64 mg/dL and that of PD patients was 5.14±1.68 mg/dL (Fig. 2E). The average parathyroid hormone (PTH) level of HD patients was 220±235 pg/mL, but the distribution of PTH levels showed extreme skewness at right tail distribution: most frequent value was about 30–100 pg/mL.
Calcium carbonate or calcium acetate was applied to 66% of HD patients, and sevelamer or lanthanum was applied to 13% of HD patients as phosphate binders. For PTH control, about 24% of HD patients were prescribed vitamin D, and cinacalcet was prescribed to only 2% of HD patients (Fig. 2F).
Miscellaneous laboratory data
The average albumin level of HD patients was 3.88±0.46 g/dL and that of PD patients was 3.52±0.51 g/dL in 2014. The average creatinine level of HD patients was 9.1±3.0 mg/dL and that of PD patients was 10.4±4.1 mg/dL. The average total cholesterol level of HD patients was 144.7±35.7 mg/dL and that of PD patients was 161.8±41.7 mg/dL. The average uric acid level of HD patients was 7.1±1.7 mg/dL and that of PD patients was 6.8±1.7 mg/dL. The average hemoglobin A1c level of diabetic HD patients was 6.9±1.5% and that of diabetic PD patients was 6.6±1.5%.
Dialysis adequacy
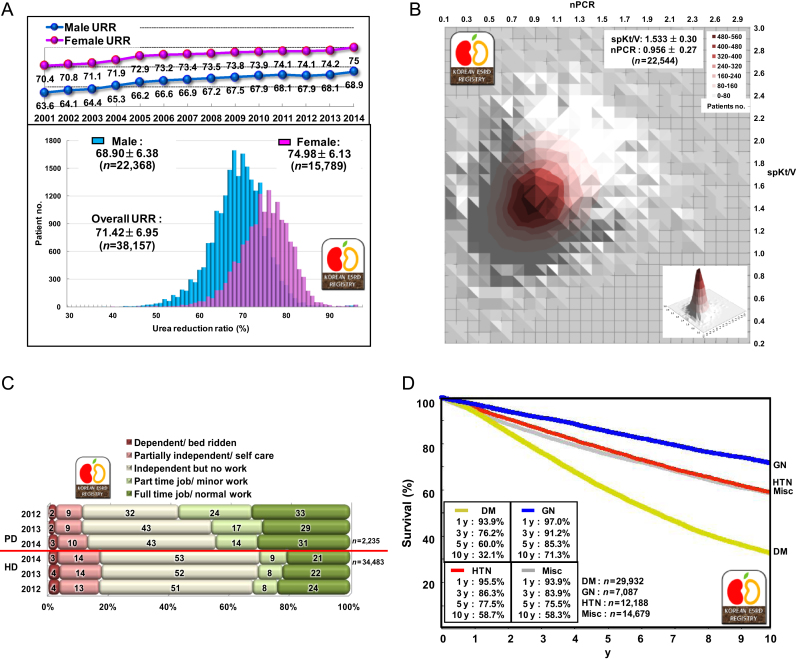
The overall urea reduction ratio of HD patients was 71.4±7.0 in 2014. The average urea reduction ratio of male HD patients was 68.9±6.4%, and that of female patients was 75.0±6.1%, which had been steadily increasing from 63.6% and 70.4% in male and female patients in 2001 (Fig. 3A). The normalized protein catabolic rate of HD patients had minimal interval change during 2001–2014 (men, from 0.90 to 0.91; women, from 1.05 to 1.02), but single-pool Kt/V had steadily increased (men, from 1.05 to 1.42; women, from 1.53 to 1.69) (Fig. 3B).
Rehabilitation, comorbidity, and causes of death
At the end of 2014, about 31% of PD patients had a full time job, but only 21% of HD patients had a full time job. On the contrary, 17% of HD patients and 13% of PD patients were dependent in daily living or bed ridden state. The most common comorbidity was reported in 2014 as vascular diseases, which was present in 48.3% of HD patients and 56.8% of PD patients. Coronary artery disease was also present in 9.3% of HD patients and 7.4% of PD patients (Fig. 3C). The most common cause of death in HD patients was cardiac (32%), and the next common cause was infection (26%). In PD patients, cardiac death occurred in 34% and death due to infection occurred in 33% in 2014.
Survival of dialysis patients
The 5-year patient survival rate since 2001 was 68.7% in men and 71.8% in women. The 5-year diabetic patient survival rate was about 60.0% (Fig. 3D).
Discussion
The size of the KSN registry data has grown 35 times in the last 30 years, in which the data on 1,800 dialysis patients in 1985 and the data on 64,000 dialysis patients in 2014 had been included [2–4]. The annual growth rate of the number of dialysis patients was as high as 9% in recent several years according to the expansion of diabetic patients and elderly population. The overall cost for dialysis has also rapidly increased; the cost in Korea was estimated to be 1,600 billion Korean won ($1.5 billion) in 2013 according to the health insurance review and assessment service report, and the cost in the USA was $34.3 billion in 2011 according to the USRDS report. A nationwide special dialysis therapy administrative bureau with dialysis patient registration program and dialysis specialist group is thought to be necessary for the adequate administration of this rapidly expanding dialysis therapy in the long-term perspective.
The population of diabetic patients is still rapidly increasing in Korea according to the Korean Diabetes Association’s survey, so the diabetic proportion of dialysis patients is expected to grow continuously during the next several years. Moreover, because diabetic dialysis patients are usually involved in multiple serious diabetic complications other than diabetic nephropathy, such as ischemic heart disease, diabetic retinopathy, and peripheral neuropathy, the care of a diabetic dialysis patient is a very huge medical burden to the medical personnel in a dialysis unit. More strict control of diabetic patients with cooperation of endocrinologists and nephrologists is necessary for the reduction of the prevalence of diabetic nephropathy.
In contrast to the rapid increase of HD patients, the number of PD patients had not increased and even decreased in the last several years. This finding was also seen in the United States, but the number of PD patients increased in some countries, such as Hong Kong and Mexico, in which PD therapy was forcefully driven by the health ministry [5]. The guidelines or recommendations on dialysis therapy choice for Korean patients will be helpful for initial dialysis modality choice.
In the aspect of dialysis facilities, the proportion of private clinics in dialysis therapy has increased. The reason is thought to be that dialysis therapy has become quite a safe and popular medical procedure, and the stable long-term dialysis maintenance patient population has increased. Another aspect of dialysis facilities was the expansion of nursing hospitals for elderly patients with dialysis centers. Recently, owing to the increase of elderly dialysis patients, hundreds of nursing hospitals started to run affiliated dialysis facilities, in which nephrologic care was often insufficient. Therefore, the continuing education and evaluation of dialysis personnel in private clinics and nursing hospitals should be mandatory.
About half of dialysis patients were under dialysis for more than 10 years. These long-term dialysis patients should be evaluated and monitored for chronic dialysis complications. Some dialysis modifications, such as HDF therapy, might be considered for the prevention of long-term dialysis complications.
Blood pressure control, anemia control, and dialysis adequacy have continuously improved in dialysis therapy in Korea. However, multiple high dose antihypertensive, high dose EPO, and expensive high performance dialyzer were needed for these improvements. The importance of calcium and phosphorus control also has been increasing according to the increase of long-term dialysis patients. However, the cost-effectiveness evaluation on these controls might be needed because of recently introduced high-priced phosphate binders, vitamin D, and calcimimetics.
The reported patient survival rate of KSN registration data was much higher than that in other countries, such as Japan and the United States. These high patient survival rates were due to low registration rate (about 70%) and missed death reports. This finding is another important reason why the KSN ESRD patient registration should be run by the KSN and health ministry together, by which the dialysis fee reimbursement should be accompanied.
Conclusion
We, the KSN ESRD registry committee, have performed the dialysis patient registration and reported for 30 years. HD patients, especially the diabetics and elderly patients, have increased in number very rapidly during recent several years in Korea. As the patient population increase, the medical cost for dialysis has also increased. To reduce this burden, diabetic nephropathy care and elderly patient care should be emphasized.
Anemia, high blood pressure, and dialysis adequacy have gradually improved by high-dose EPO therapy, multiple antihypertensives, and high performance dialyzer, respectively, but the cost-effectiveness of these therapies should be evaluated. Because the long-term dialysis patient population has increased, chronic dialysis complications should be closely monitored and dialysis modifications, such as HDF therapy, might be considered. Because of the increase of private clinics and nursing hospitals in dialysis practice, the role of the dialysis specialist and continuing education are thought to be essential.
For strict cost-effective dialysis control of increasing elderly, diabetic, and long-term dialysis patients, the KSN ESRD patient registration should be run jointly by the KSN and health ministry, by which the dialysis fee reimbursement should be accompanied.




 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print
















